Background: Moonlighting trainees are an essential labor source for expanding hospital medicine groups. Though the ACGME specifies moonlighting eligibility criteria and duty work hour restrictions, it does not address specific onboarding requirements. Prior to this project, our section of hospital medicine had no formal onboarding process for moonlighters despite 400-500 shifts covered annually by approximately 90 internal medicine residents and fellows. The absence of a structured onboarding process results in a lack of adherence to standardized documentation practices such as H&P templates, IPASS handoff and a lack of knowledge of hospitalist patient management. Standardized documentation and handoff are associated with improved patient safety and medical error reduction.
Purpose: The aim of this project is to develop and implement an onboarding curriculum for moonlighters to increase standardized H&P and IPASS documentation and increase hospitalist patient management knowledge to improve patient safety.
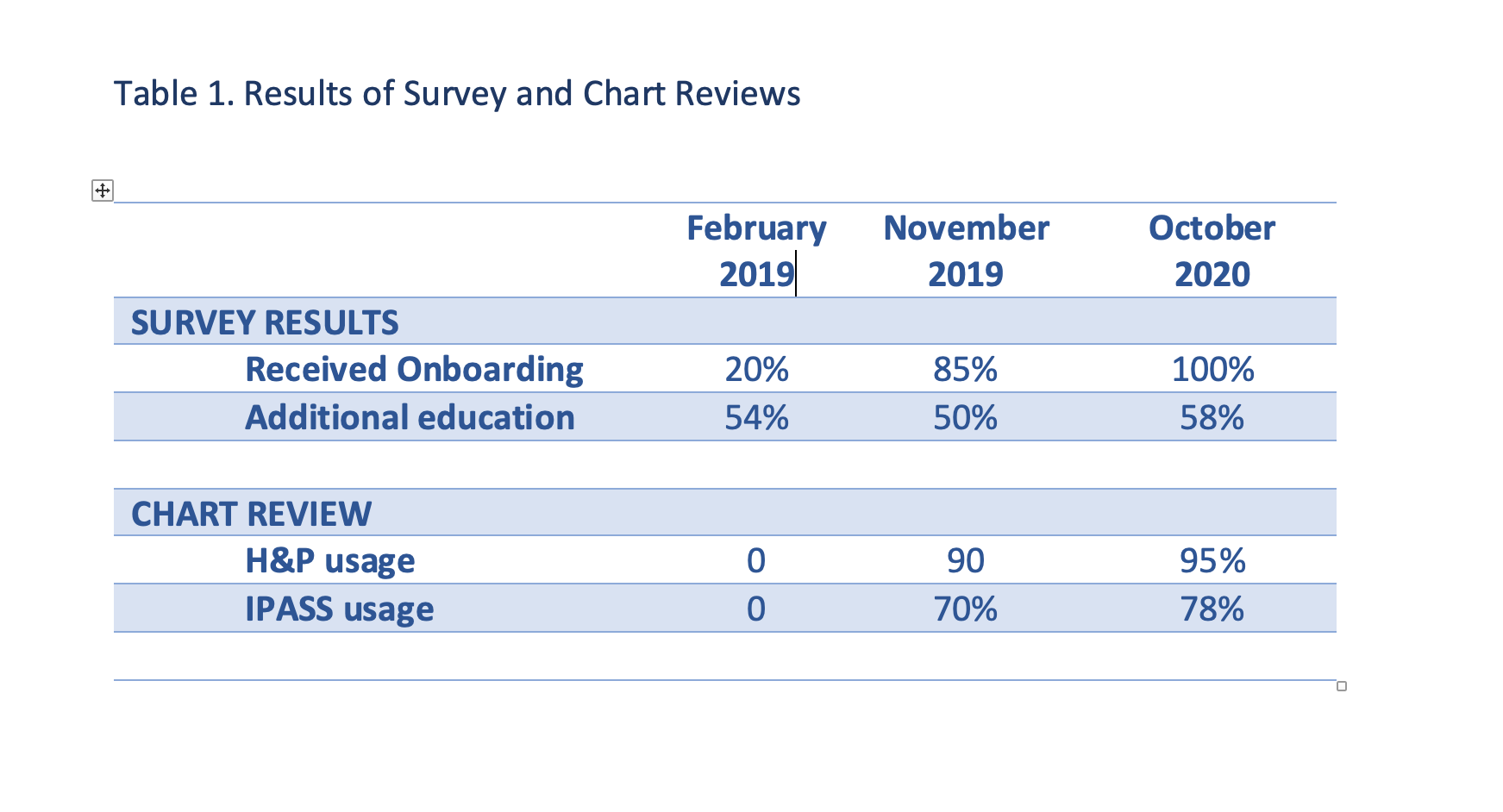
Description: In early 2019, an onboarding curriculum was developed based on the results from a pre-intervention survey sent to eligible residents and fellows and a chart review of standardized IPASS and H&P documentation performed by the night director. Only 20% of respondents reported receiving onboarding and 54% of respondents requested additional education for managing hospitalist patients. Of the 144 charts reviewed, no moonlighters used standardized H&P or IPASS documentation (Table 1). One hour in person mandatory onboarding sessions were offered in July and August of 2019. A six month follow up survey revealed 85% of respondents reported receiving onboarding and 50% wanted additional education for managing hospital medicine patients. Of the 177 charts reviewed 6 months after onboarding, H&P documentation increased to 90% and IPASS use increased to 70%. In July 2020, onboarding shifted to one hour live video sessions due to COVID restrictions. Only second year residents, new fellows and those who had not completed previous onboarding were required to complete this training. All moonlighters were expected to review updated onboarding materials on a newly created shared drive containing educational materials, onboarding slides, COVID resources and hospital system information. Biweekly emails were also initiated to provide clinical updates and reinforce documentation expectations with emphasis that adherence to hospital medicine standardized documentation is necessary for moonlighting eligibility. A follow up survey sent in October 2020 to all moonlighters revealed 100% of respondents received onboarding and 58% wanted additional education on managing hospitalist patients. Of the 170 charts reviewed, H&P documentation increased to 95% and IPASS usage increased to 78%.
Conclusions: A structured onboarding curriculum consisting of one hour training sessions, a shared drive and email communications improved moonlighter adherence to standardized H&P and IPASS documentation. Despite these interventions, moonlighters requested additional education on hospitalist patient management. This may be unique to our hospital as our hospitalists manage liver, renal and lung transplant patients. Though additional assessment is needed to understand the education requests, transplant was identified across time in the surveys as a specific area for more education.