Background: Lumbar puncture (LP) is commonly needed in hospitalized patients for both diagnostic and therapeutic purposes. Traditional landmark identification by palpation of the lumbar spine and pelvis often has a low success rate. There is strong evidence showing that the use of ultrasound leads to higher success rates, along with other important patient-centered outcomes such as a reduced time to LP, fewer needle passes, and lower rates of traumatic LP. Since 2016 the University of Minnesota has had an active Bedside Procedure Service (BPS), with highly trained hospitalists performing bedside LPs for the entire hospital. At inception, use of ultrasound during lumbar puncture was varied amongst the BPS group. Due to evidence of increased success, we elected to standardize the sagittal-oblique paramedian (PM) approach among all BPS faculty. Success rates between different approaches to LP and the impact of standardizing the use of ultrasound amongst such a group are not well described. This study aims to assess the impact of standardizing a new approach to bedside LP.
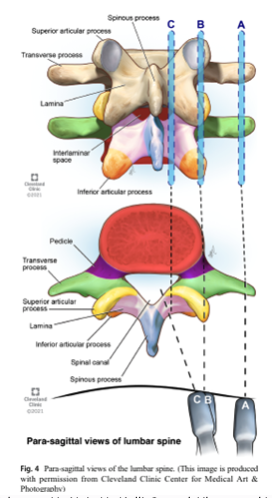
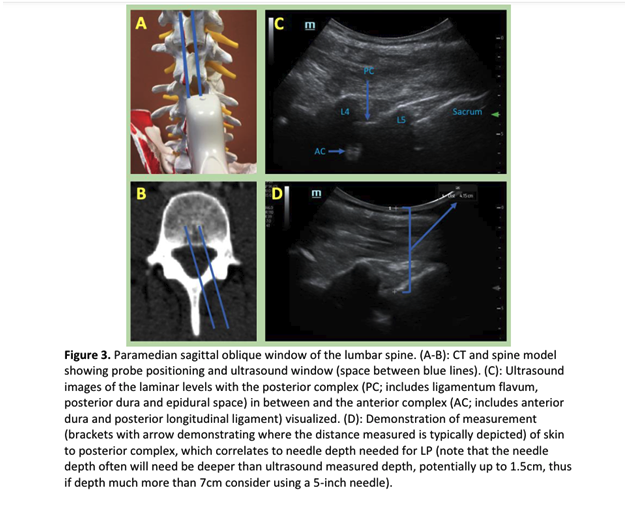
Methods: The initial ultrasound technique using the PM approach was utilized by a single hospitalist in 2018 after intensive self study and training with anesthesiology. After developing and standardizing a curriculum (consisting of images and text on a cloud-based server), each BPS member was given access to the curriculum for self-study and received at-the-elbow instruction on the PM approach until competency was reached. This was demonstrated by 2-3 independently successful LPs using a PM approach. The date each BPS member became competent using the PM approach was recorded. To assess the impact of standardization, all LPs performed from October 2017-May 2022 were reviewed. All procedures attempted by BPS faculty at the University of Minnesota were recorded, including whether or not the procedure was successful, the date the procedure was performed, and the individual performing the LP. Data were then abstracted before and after the training sessions for each faculty member to compare success rates. The primary outcome was the overall success rate of the BPS before and after each hospitalist became competent in the PM approach.
Results: Between 10/6/2017 and 5/5/2022 the BPS attempted a total of 467 LPs by 20 different BPS faculty. Of these, 162 were performed prior to the standardized use of the PM approach and 307 were performed afterwards. The unadjusted overall success rate for bedside LP before the intervention was 72.8% and 87.5% afterwards (P-value < 0.0001). The unadjusted odds ratio for a successful LP after the standardized use of the PM approach was 2.6 (CI 1.6-4.2). Using a mixed-methods analysis to control for patient and proceduralist related factors yielded similar results with an OR of successful LP of 2.6 (CI 1.6-3.6) . Secondary outcomes including the number of attempts, success rates by inter-spinal space, and rates of traumatic LP are being explored.
Conclusions: Through a semi-formal educational intervention, the BPS at the University of Minnesota significantly improved the rate of successful bedside lumbar puncture using the PM approach. This led to the development of a formal curriculum and suggests that for vast majority of hospitalized adults, ultrasound-assisted LP should first be attempted using the PM approach. Important topics of future study should include the comparison of the PM approach with other ultrasound assisted approaches and the impact of incorporating a formal curriculum into Internal Medicine training.