Background: Statin use has been shown to be beneficial in secondary stroke prevention. However, the optimal LDL level that should be achieved is still uncertain. Since there is a dearth of information, it is unclear if statins are useful in patients with stroke with baseline LDL ≤70 mg/dl in terms of morbidity and mortality outcomes.
Methods: This is a prospective single-center observational study including adult patients hospitalized for a stroke with LDL ≤ 70 mg/dl on index admission between Jan 2021 to Oct 2022. Baseline characteristics were collected by reviewing electronic medical records. We excluded patients aged < 18 years and stroke due to traumatic event. Based on statin use before index admission, patients were divided into: Group A: already on statin; Group B: statin naive. Follow-up calls were made at 6,12 and 18 months after discharge. We compared the incidence of mortality, readmission rates, and Modified Rankin Scale (MRS) scores between the two groups.
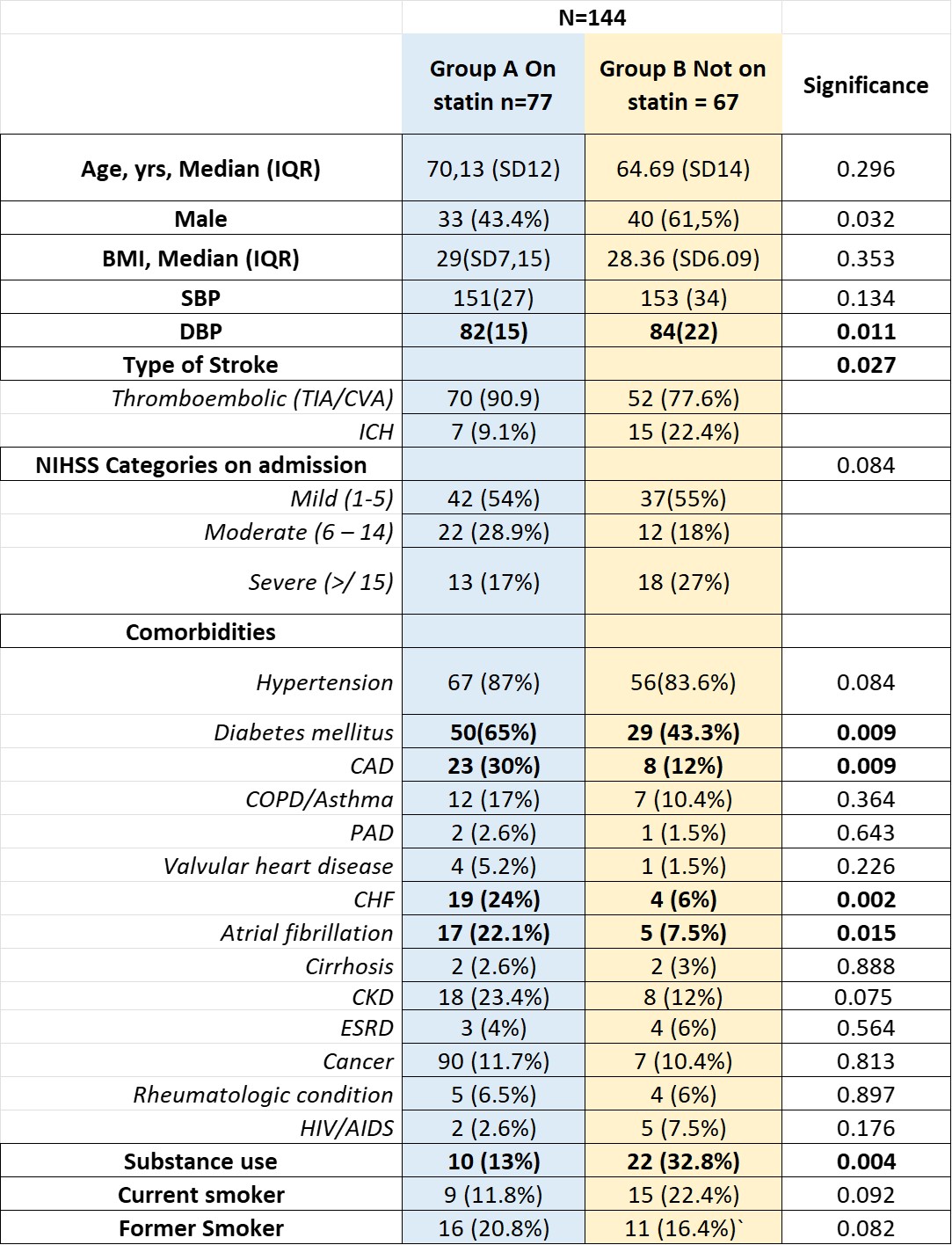
Results: Out of 614 patients admitted for stroke, 144 (23%) had LDL ≤70 mg/dl. Before index admission, 77 were already on a statin (group A), while 67 were statin naive (group B). The prevalence of known coronary artery disease, atrial fibrillation (AF), and heart failure (HF) was higher in group A, while substance use was higher in group B (table 1). The cumulative incidence of ischemic stroke in group A was 90.9% versus 77.6% in group B. Incidence of hemorrhagic stroke was significantly lower in Group A; 9% vs. 22.4% in statin naïve patients (p=0.02, OR 0.314 CI95% 0.132-0.911). This difference remained significant in the subgroup of admission systolic blood pressure (SBP) >160 between both groups A/B; lower incidence of hemorrhagic stroke vs. ischemic (p=0.007). Inpatient mortality was lower in group A than in group B; (10.4% vs. 17.9%, p=0.159). The difference also became significant in patients age < 65 with higher mortality seen in Group B (p=0.041). Moreover, the mean MRS at discharge was minimally different but significant, 3 vs. 2.9 (p=0.004). We received responses from 36, 30 and 17 patients at 6, 12 and 18 months, respectively. All-cause mortality at 6 months is 11% with a higher mortality seen in patients who were not discharged on statins (40% vs 6.5% p=0.027). There is an overall higher readmission rate during the first six months, 58% out of which 28% was due to recurrent stroke.
Conclusions: The results demonstrate a positive association between the use of statins and overall better morbidity and mortality outcomes. We observed a lower incidence of hemorrhagic stroke in group A and subsequently less mortality on index admission. People aged < 65 who were statin naive had higher mortality than older patients during index admission. Our subgroup analysis manifesting higher mean SBP on admission, did not correlate with higher incidence of hemorrhagic stroke; therefore, an independent benefit of statin can be associated to the type of stroke. Although limited by sample size, a significantly increased incidence of mortality at 6 months is noticed in statin naive patients. We observed better functional status on discharge with overall lower mortality and morbidity at 6-18 months follow up in patients taking statin.These results are mostly consistent with other cohorts that have reported that a goal LDL of < 70 mg/dl has a decreased risk of recurrent CV events following an ischemic stroke or TIA with evidence of atherosclerosis than those with a target range of 90 to 100 mg/dl, our data is unique in analyzing the patients who have already achieved goal LDL < 70 mg/dl before stroke.