Background: The underlying burden of medical co-morbidity is often the main driver of ICU transfer of patients initially admitted to the medical wards (1). The role of non-patient related factors is unclear, as are the mortality and economic data associated with ICU transfer from the medical ward. The purpose of this analysis was to identify the demographic and clinical characteristics associated with unplanned medical intensive care unit (MICU) admissions of patients admitted to medical wards, and to describe the clinical and economic outcomes associated with unplanned MICU admissions.
Methods: This retrospective matched cohort analysis utilized the PINC AI Healthcare Database, which represents approximately 25% of all US inpatient admissions. Discharge records were assessed for admissions in 2021, and billing lines were used to identify patient care floor locations and unit transfers. Inclusion criteria were: Age ≥18 years and medical/surgical or telemetry care floor utilization. Unplanned MICU admission was defined as a direct transfer from a medical or telemetry care floor to the MICU. Propensity score matching was performed to match medical patients with and without unplanned MICU admission 1:1 within each Medicare Severity Diagnosis Related Group. Differences in patient characteristics and outcomes between patients with vs without unplanned MICU admissions were assessed using two-sample t-tests for continuous measures and Chi-square tests for categorical measures.
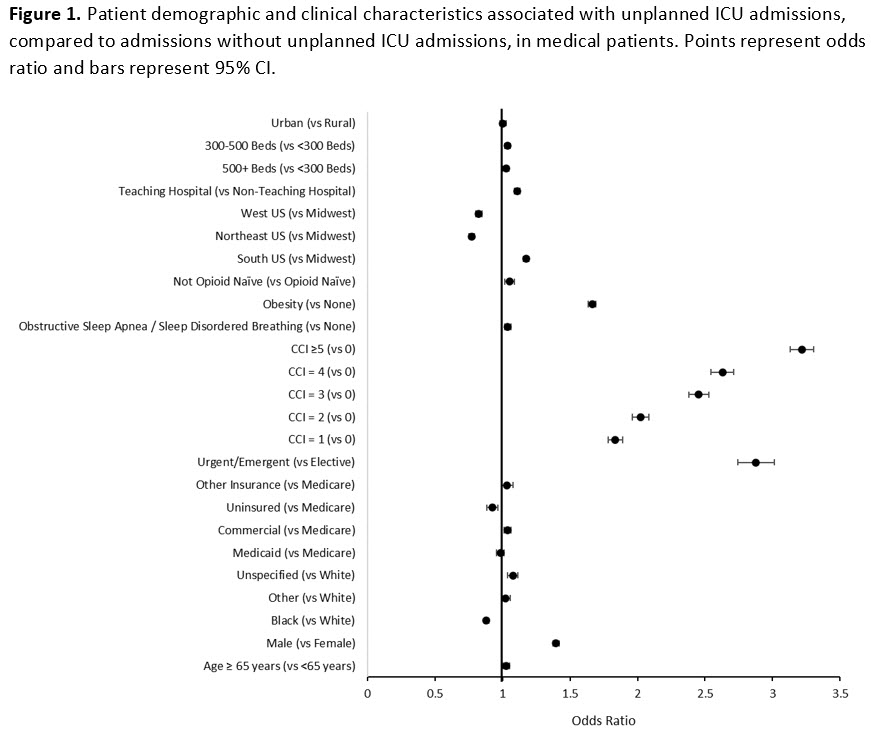
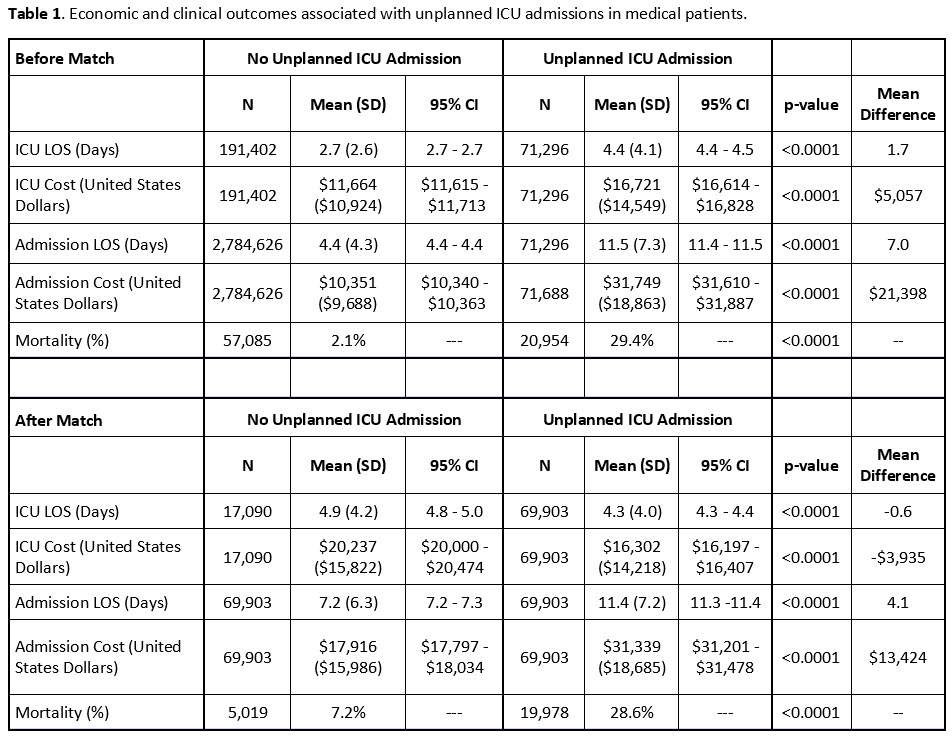
Results: A total of 2,855,922 medical admissions were assessed. Of these admissions, 71,296 (2.5%) had unplanned MICU admissions. Patients under 65 represented 45% of hospital admissions with unplanned MICU admissions and 55% of hospital admissions without unplanned MICU admissions. Hospital admissions with unplanned ICU admission were more likely to be urgent/emergent (odds ratio [OR] 2.9, 95%CI 2.7-3.0, p< 0.001), male (OR 1.4, 95%CI 1.4-1.4, p< 0.0001) and have obesity (OR 1.7, 95%CI 1.6-1.7, p< 0.0001). Compared to patients with a Charlson Comorbidity Index (CCI) of 0, the odds of unplanned ICU admission increased as the CCI increased from 1 (OR 1.8, 95%CI 1.8-1.9, p< 0.001) to ≥5 (OR 3.2, 95%CI 3.1-3.3, p< 0.001) (Figure 1). After matching, 69,903 admissions were included in each cohort. Between matched patients with and without unplanned MICU admission, the mean difference in total admission length of stay was 4.1 days (p< 0.001) and the mean difference in total admission cost was $13,424 (p< 0.001). In the unmatched population, mortality rates were 29% and 2% in patients with and without unplanned MICU admission, respectively (p< 0.001). After matching, mortality rates in patients with or without unplanned ICU admission were 29% and 7%, respectively (p< 0.001) (Table 1).
Conclusions: Patients with higher burden of medical morbidities and obesity initially admitted to the medical wards are more likely to require ICU level care. These patients often continue to have higher mortality and cost of care after transfer to the MICU.