Background: As inpatient medical care has increased in complexity and fragmentation, rounding has become siloed away from patients and by discipline, resulting in disjointed and inefficient care models. In response, hospitalist groups across the country have been implementing unit-based rounding programs to centralize communication and align work-flow of health care team members. At UC San Diego Health, the Division of Hospital Medicine rolled out FIT (Focused Interdisciplinary Team) Rounding in 2017 across seven diverse patient care units. Since implementation, we have been working to maintain standardization of rounding behavior and track the impact of FIT on care quality and efficiency.
Purpose: We aimed to design a user-friendly electronic medical record (EMR) embedded tool to track elements of rounds discussion and quality measures in real-time. Data from this flowsheet can be leveraged for three purposes: 1) remotely assess FIT rounding fidelity across multiple units, 2) evaluate the direct impact of FIT on patient flow elements, and 3) track direct impact on quality metrics.
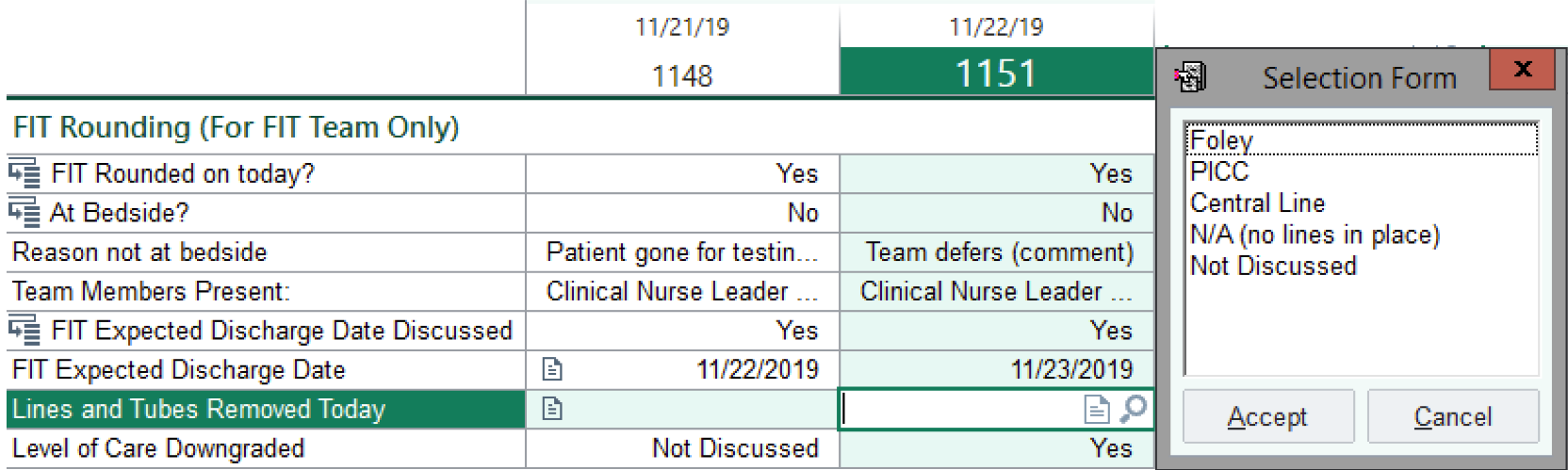
Description: We created a flowsheet in the EMR (figure 1) to document elements of FIT rounds discussion that were determined to be most valuable. With simple drop-down lists, the user identifies: 1) whether or not FIT rounds had been done that day, 2) whether or not rounds were done at the patient’s bedside, 3) which team members were present, 4) whether or not the expected discharge date had been discussed, 5) which lines and tubes were removed, and 6) whether or not the level of care had been downgraded. If FIT rounding was not done at bedside, a drop down list would appear providing options for why bedside rounding did not occur (patient was on contact/droplet/airborne precautions, patient was non-English speaking, patient was not present in the room, patient was gone for testing/treatment, patient deferred, team deferred). If the expected discharge date was discussed, a calendar would appear facilitating the selection of the expected discharge date. The FIT Rounds Interdisciplinary Leadership team appointed the rounds coordinator to use a computer station on wheels and populate the flowsheet fields during rounds. The flowsheet was piloted on an oncology/palliative care unit. According to user feedback, the FIT Flowsheet is easy to use, does not distract from FIT rounds, and empowers the clinical nurse leader to ask about quality metrics on rounds and ensure that they are routinely addressed. With this tool, we can remotely track fidelity elements of FIT rounding, such as patient and team member involvement, across multiple units simultaneously. Additionally, quality outcomes, such as Foley utilization and central line removal, can be directly linked to our rounding program. The tool itself may also increase adherence to discussion check lists. Preliminary data shows improved level of care utilization and a trend toward shortened length of stay since implementation of the flowsheet.
Conclusions: A simple, click-based flowsheet in the EMR to document key elements of interdisciplinary rounding discussion empowers rounds coordinators and facilitates rounding fidelity. The data collected by this tool can also be used to inform staff re-education efforts and assess the impact of multidisciplinary rounding on quality care metrics. As we continue to transform inpatient healthcare delivery for improved efficiency and quality, harnessing the EMR to track and sustain innovations will be critical in driving value-based care.