Background: Self-directed discharge, also known as Against Medical Advice (AMA) discharges, comprise 1–2% of hospital discharges (1). The AMA process poses safety risks to patients and emotional strain on providers, potentially leading to implicit biases in documentation (2). While stigmatizing language in medical records has gained attention (3), its prevalence in AMA documentation remains underexplored. This study identifies stigmatizing language in AMA discharge notes and suggests neutral alternatives.
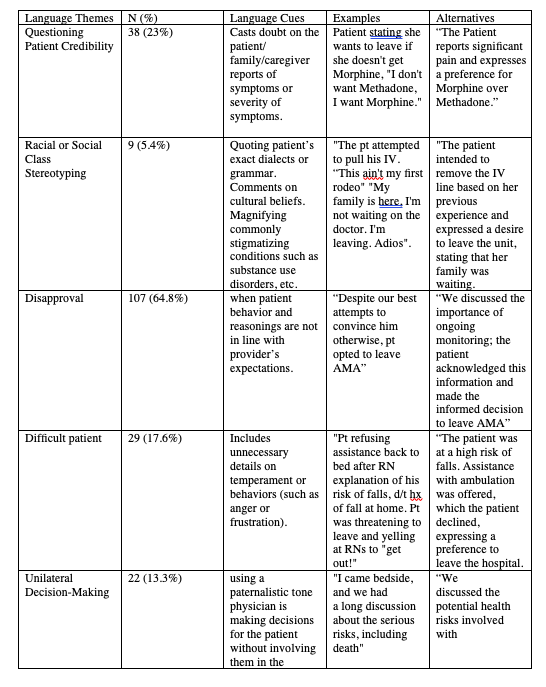
Methods: Using the electronic health record, we identified 1126 discharges designated as discharge disposition of “Against Medical Advice” between 2017 and 2023. Every 6th case was selected for review, yielding 165 patients who self-directed their discharge. This designation is made by the discharging nurse. Physician and nurse documentation surrounding the discharge was analyzed for stigmatizing language based on a framework adapted from 2 large recent studies on stigmatizing language in documentation (4, 5). Language themes were categorized into five domains: questioning patient credibility (providers doubt with patient’s report of symptoms), disapproval (statements about patient’s poor reasoning or decision making), difficult patient (unnecessary details on temperament or behaviors or direct quoting of patients’ strong language), unilateral decision-making (using a paternalistic tone without involving the patients in the conversation), social stereotyping (statements about social, sexual, racial, substance use stigmas). Two physician reviewers independently entered coded data into RedCap, with a third reviewer resolving discrepancies. For each identified instance, reviewers suggested neutral alternatives.
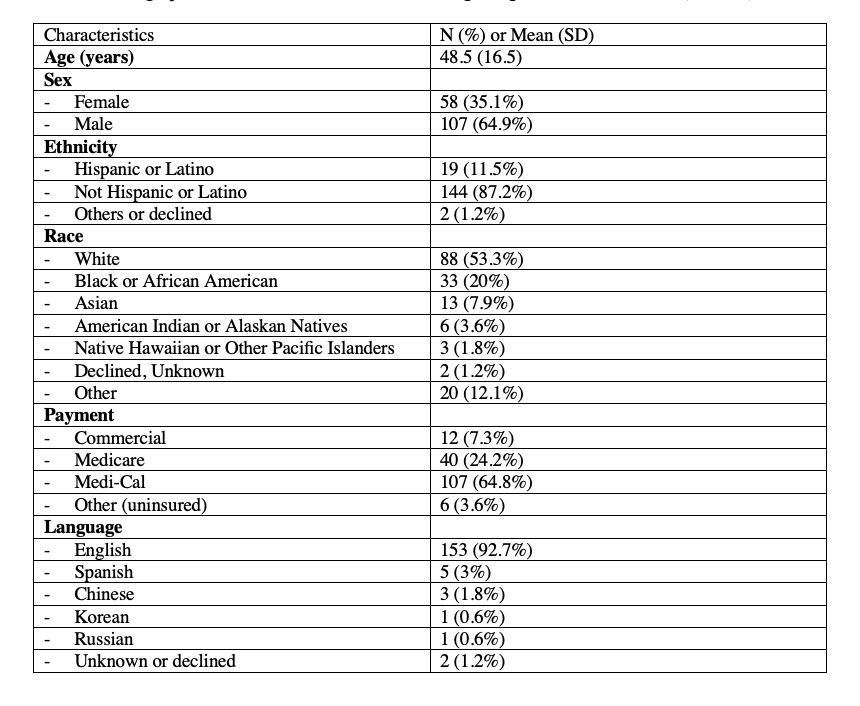
Results: Demographic data regarding the selected patients is summarized in Table 1. The mean age of patients was 48.5 years, and 107 (64.9%) were male. Stigmatizing language was more prevalent in physician notes (64.8%, 107 cases) compared to nurse notes (52.1%, 86 cases). Physicians used the term “AMA” in 81% of notes, compared to 17% using neutral alternatives like “self-directed discharge.” Similarly, nurses used the term “AMA” in 89% of cases, with neutral terms used in 11%. Potentially stigmatizing language instances were identified in 136 charts (82%) (Table 2). The most frequent theme was disapproval, identified in 107 cases (64.8%). Difficult patient narratives appeared in 53 charts (32.1%), while unilateral decision-making language was found in 22 charts (13.3%). Instances of social stereotyping were rare, identified in 9 charts (5%).
Conclusions: This study highlights the high prevalence of potentially stigmatizing language in self-directed discharge documentation, with the disapproval of patients’ decisions and difficult patient narratives being the most common themes. Raising awareness of implicit biases in clinical documentation is critical to reducing the use of stigmatizing language and its potential negative impact on future patient care. Limitations include the small sample size, underscoring the need for larger studies with control groups to better understand how stigmatizing language affects patient outcomes. Future research should prioritize the development of targeted interventions and neutral language models to promote unbiased, patient-centered documentation practices in healthcare settings. This may need to be balanced against priorities of accurate representation of threats to staff safety.