Background: The use of maintenance fluids (MF, continuous intravenous fluid (IVF)) to prevent dehydration is common, yet highly variable in practice. Unnecessary MF can cause patient harm including fluid overload, sleep disruption (associated alarms), and increase falls risks. In 2017, Hurricane Maria destroyed Puerto Rican facilities that were critical in producing IVF, exacerbating an existing shortage of IVF in the US.
Purpose: In this quality improvement project, we conducted an interdisciplinary, multifaceted intervention to reduce MF overuse on hospitalist services.
Description: At an urban, tertiary care, academic hospital, we implemented an interdisciplinary intervention to reduce unnecessary MF use among 6 teaching and 5 non-teaching teams led by hospitalists. This included: (1) education and publicity campaign, (2) targeted feedback, and (3) EMR changes.
The education and publicity campaign incorporated current guidelines (NICE, 2017) for MF. We conducted educational sessions for residents, advanced practitioners and physicians at noon conferences and block orientations, and for bedside nurses at daily huddles. Informational cards on nurse and clinician workstations had the slogan, “Stop the Flow if Your Patients PO” to prompt reassessment of MF for patients who could take oral fluids. We encouraged nursing staff to feel empowered to tell clinicians when patients on MF could take oral fluids. The second strategy used targeted feedback via a HIPAA-compliant texting application, with friendly reminders to attendings to reassess MF use when MF were given for >48 hours and >72 hours in patients who were not NPO. Finally, EMR (Epic) orders were changed to set a default 72-hour limit on continuous IVF (with option to override), with a nonintrusive advisory warning reminding clinicians of the critical IVF shortage.
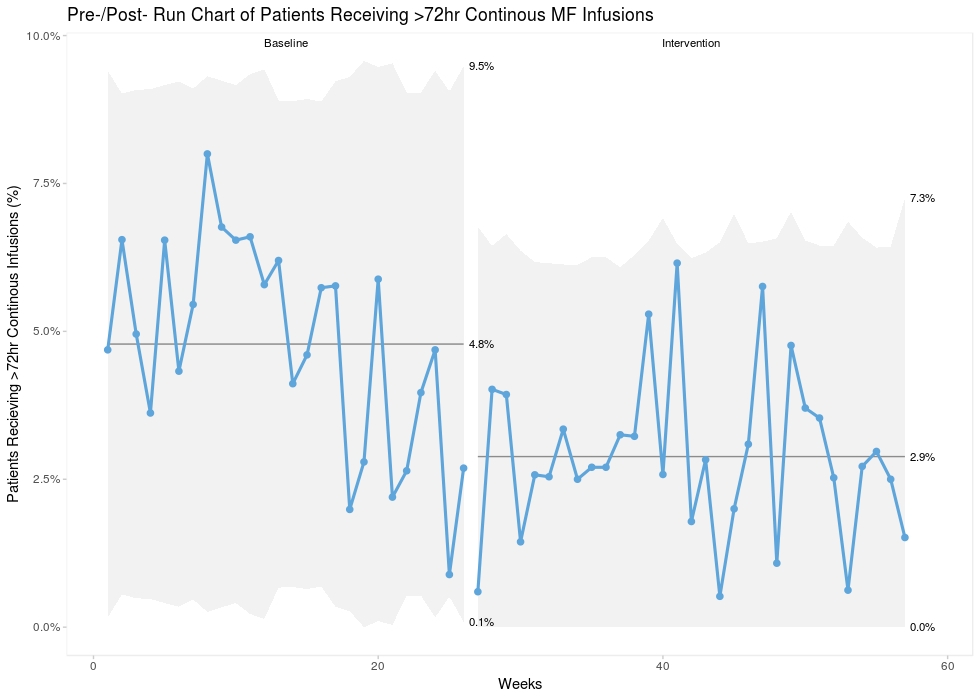
Pre-intervention data (July – December 2017) was collected from EMR and compared to post-intervention (January – August 2018). MF were defined as 0.9% NaCl, 5% dextrose in 0.45% NaCl, 5% dextrose, plasmalyte, and lactated ringers at rates of 50-150 cc/hour for greater than 12 hours. The difference in MF utilization was assessed using a two-sample t-test. The volume of MF decreased from 746.6 L/mo to 607.8 L/mo (p=<0.001). The percent of patients receiving MF for >72 hours decreased from 4.8% to 2.9% (p=<0.001) and the percent of patients who received MF for >24 hours decreased from 18.3% to 15.6% (p=<0.01).
Conclusions: Using a robust, interdisciplinary, multifaceted approach based on education and publicity, targeted feedback, and EMR system changes, we successfully reduced MF prescribed on 11 hospitalist teams. The identification of MF overuse as an actionable target is relatively new to the medical literature. This project may serve as a model for other institutions to identify and decrease MF use.