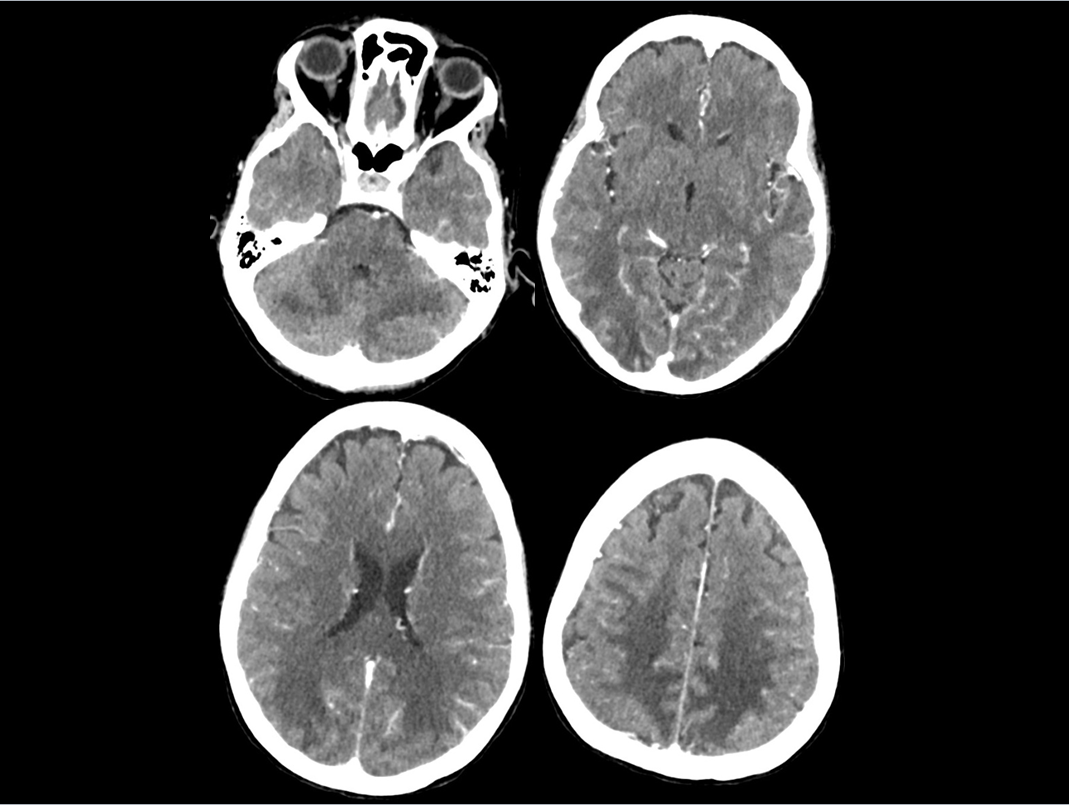
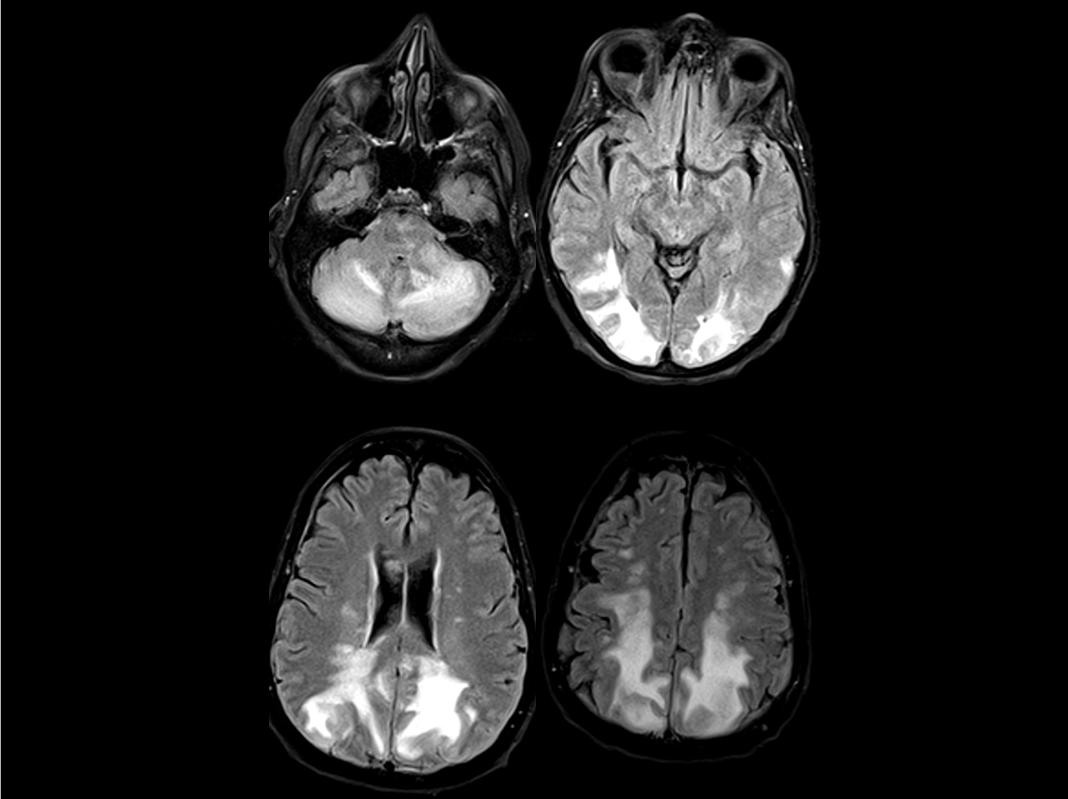
Case Presentation: A 67 year old female patient with diffuse large B-cell Lymphoma with extensive nodal disease involving the lower thorax, abdomen, pelvis and central nervous system (CNS) presented with generalized weakness, acute confusion and fevers. Her recent treatment history included systemic chemotherapy with dose adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, rituximab (DA-EPOCH-R) and intrathecal chemotherapy with methotrexate (MTX) which she had received for the first time three days prior to presentation. During the initial assessment she was febrile with temperature of 103 F but was otherwise hemodynamically stable. She denied nausea, vomiting, diarrhea, chest pain, or shortness of breath. Abruptly, she complained of acute vision loss bilaterally with a subsequent witnessed grand mal seizure. She was intubated and started on propofol as she had severe hypertension. CT of the head demonstrated bilateral and symmetrical vasogenic edema in the right and left posterior frontoparietal and occipital cortex and cerebellar hemispheres [Image 1]. MRI of the brain showed vasogenic edema in the cerebellum and parieto-occiptal lobes with no restricted diffusion consistent with posterior reversible leukoencephalopathy syndrome (PRES) [Image2]. Electroencephalogram (EEG) showed diffuse nonspecific moderate encephalopathy. She was started on levetiracetam 1500mg BID and lacosamide 100 mg BID. Routine EEGs performed revealed occasional generalized periodic discharge (GPDs). It was felt the PRES was secondary to DA-EPOCH-R with hypertension. She was monitored in the hospital for thirteen days and post discharge had significant clinical improvement with optimal blood pressure management.
Discussion: Reversible posterior leukoencephalopathy syndrome (PRES) first mentioned in 1996 is a clinical syndrome consisting of headache, confusion, visual changes, seizures and associated neuroimaging findings of posterior cerebral white matter edema. The pathogenesis appears to be related to cerebral autoregulation and endothelial dysfunction. The failure of normal auto regulatory mechanisms in the maintenance of cerebral arteriolar pressure causes sudden hyper perfusion and extravasation of fluid leading to edema in the white matter of the brain. It has been hypothesized that increased numbers of adrenergic nerves in the posterior white matter leads to prevalence in the posterior aspect of the brain. Essential to the diagnosis of PRES is timely neuroimaging consisting of CT followed by brain magnetic resonance imaging. Treatment of PRES involves symptomatic management of hypertension and seizures along with discontinuation of offending agent or condition such as pregnancy, etc. Most cases improve in few weeks after termination of offending factor and control of blood pressure.
Conclusions: PRES can result from various etiologies of which hypertensive encephalopathy, thrombotic thrombocytopenic purpura, and eclampsia are common. In rare occasions, it also occurs in electrolyte imbalance and sepsis. Common chemotherapeutic agents such as are vincristine, rituximab and gemcitabine can cause PRES. This case serves to raise awareness amongst hospitalists that PRES should be a differential diagnosis in the setting of patients receiving certain chemotherapeutic agents presenting with the aforementioned clinical symptoms.