Case Presentation:
A 22‐year‐old previously healthy woman presented in May 2008 describing fever, fatigue, diarrhea, and dysuria for 1 week. She recalled a tick bite 3 weeks prior to her illness. She was prescribed trimethoprim‐sulfamethoxazole for a presumed urinary tract infection as an outpatient. Her symptoms failed to improve, and she was admitted and diagnosed with pyelonephritis. Her temperature was 103°F, and her exam demonstrated diffuse muscular weakness and mild peripheral edema. She had a WBC of 2400/μL, a platelet count of 27,000/μL, an ALT of 567 units/L, an AST of 1623 units/L, and a creatinine of 1.6 mg/dL She developed acute respiratory distress after several days and required transfer to the ICU. She remained febrile and her condition continued to worsen despite treatment with broad‐spectrum antibiotics. Doxy‐cycline was added for suspected tick‐borne illness, and her symptoms and laboratory abnormalities resolved within a few days. Extensive infectious and rheumatologic etiologies were explored which revealed a positive IgG serology for Ehrlichiosis chaffeensis 1:256 (normal < 1:64).
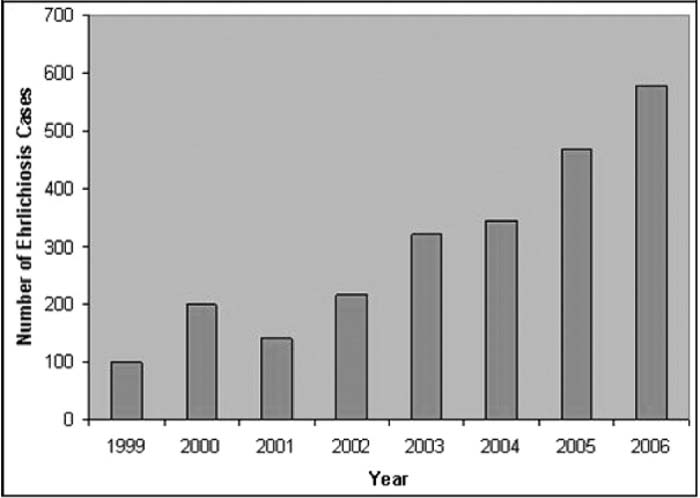
Number of ehriichiosis cases (caused by Ehrlichia chaffeensis) reported to the CDC by state health departments, 1999–2006.
Discussion:
Ehriichiosis in the Western hemisphere is a newly described illness, with its first diagnosis in 1987. Human mono‐cytotropic ehriichiosis (HME) is a systemic illness cause by a tick‐borne, gram‐negative obligate intracellular bacterium. E. chaffeensis is usually found in the southeastern/south‐central United States and is transmitted by the Lone Star tick. The clinical manifestations include fever, fatigue, myalgias, and headaches with leukopenia, thrombocytopenia, and transaminitis. Early diagnosis and treatment are important to those infected with HME. More than half receive alternative diagnoses initially. Hospitalization is required in 56% of HME infections, and the mortality rate is 3%. It is therefore important for clinicians who work in the inpatient environment in endemic areas to recognize potential HME infections. Diagnosis is made by strong clinical suspicion, serology, PCR, or buffy coat exam for morulae. The treatment of choice is doxycycline. Sulfonamide use may indicate a more fulminant course and the possibility of acute respiratory distress syndrome and respiratory failure.
Conclusions:
Often HME infections require hospital admission and multispecialty evaluation. History and physical examination are crucial, as confirmatory laboratory testing takes days to return. The associated deterioration in clinical status with sulfonamides has been noted in several pediatric case reports. The use of sulfonamides and a change in clinical course can be used as a diagnostic clue to indicate possible HME infection. It is reasonable to suggest that in endemic areas and during peak seasons, questioning about recent tick exposure should precede the prescribing of sulfonamides to avoid potential fulminant illness.
Author Disclosure:
A. Dickerson, none; D. Schulman, none.