Case Presentation:
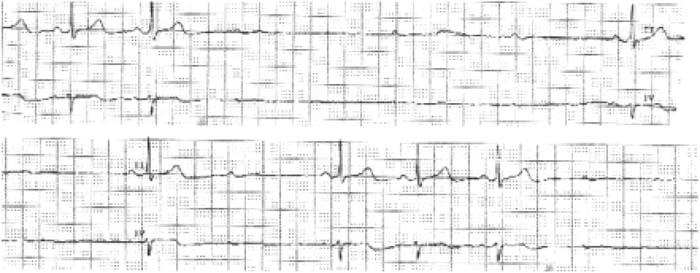
A 52‐year‐old female was admitted for the evaluation of recurrent atypical chest pain. Outpatient nuclear stress testing had suggested modest but reversible ischemia. Past medical history includes PTSD, depression, anxiety, GERD, hypertension, and hyperlipidemia. Her medications on admission included aripiprazole, furosemide, Zolpidem, venlafaxine, ibuprofen, amitriptyline, hydrocodone‐acetaminophen, hydrochlorothiazide, metoprolol, and potassium chloride. Review of systems was positive for dyspnea on exertion, chest pain, heartburn, anxiety, depression, and near syncope. Blood pressure was 159/84 mm Hg, pulse 69 bpm, and 20 respirations per minute. Exam was normal. Complete blood count, comprehensive metabolic panel, and cardiac enzymes were negative. An admission electrocardiogram showed normal sinus rhythm. Coronary angiography showed no evidence of coronary artery disease with an ejection fraction of 60% Prior tc the patients' transfer to psychiatry, she began To have episodes of transient second degree, Type II heart block and near syncope. On further questioning, these episodes occurred only while the patient was swallowing foods of a substantial consistency such as steak or chicken at the lime of the telemetry changes. The symptoms were reproducible and the episodes lasted 4‐5 seconds each. During these episodes, her blood pressure was 86/59 mmHg, pulse of 65 bpm, and oxygen saturation of 95% on room air. The patient reported that she had been having similar episodes while swallowing similar foods at home for some time. Amitriptyline was discontinued and the patient was started on a full liquid diet and symptoms resolved.
Discussion:
Discovering a unique etiology to a commonly encountered medical condition such as syncope requires obtaining a good history and physical examination. In this case. Telemetry monitoring lead directly to the diagnosis of swallow syncope. An exact mechanism behind swallow syncope is not defined but an exaggerated vagal response leading to cardiovascular inhibition is believed to be largely responsible. Most cases reported have shown some type of esophageal or cardiac abnormality on further testing. Moreover, the consistency and temperature of the swallowed food appears important. Although syncope is a common presenting complaint, swallow syncope is a rare condition that may be discovered with a thorough examination, proper diagnostic workup, and high level of clinical suspicion.
Conclusions:
Syncope is a commonly encountered problem for internists and cardiologists and often results in hospital admission and a large diagnostic workup. Unfortunately a cause is only discovered in about 30%‐40% of cases when vagal mechanisms are considered.
Author Disclosure:
J. Foreman, none; R. Wardrop, none; A. Vigh, none.