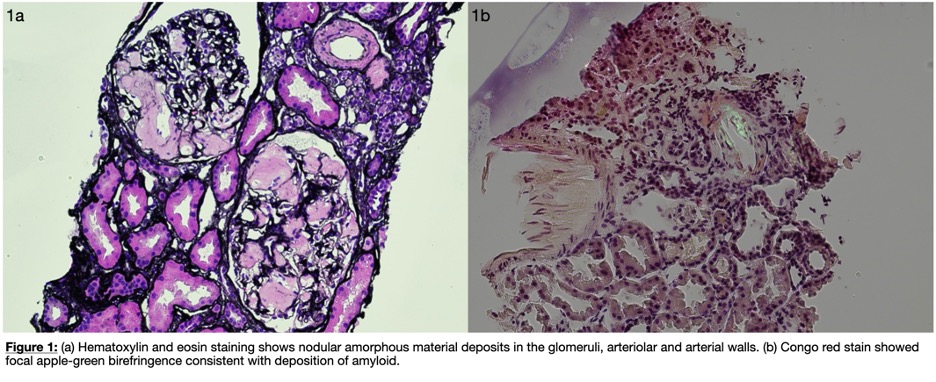
Case Presentation: A 50-year-old male with a history of hidradenitis suppurativa (HS) presented after abnormal outpatient lab work including a newly elevated creatinine. The patient has been in his usual state of health and was recently started on prednisone 30mg for his HS. In preparation for initiation of immunologic agent for HS, he went to his primary doctor who drew bloodwork, which revealed elevated creatinine to 1.74 mg/dL, hemoglobin of 8.7 g/dL, mild leukocytosis of 16,980 cells/µL, sodium of 128 mmol/L, and a significant protein gap. The patient was sent to the hospital for further evaluation. Urine protein-to-creatinine ratio was elevated at 3.9. Creatinine fluctuated between 1.7-1.9 mg/dL. Renal ultrasound showed mildly enlarged kidneys bilaterally with heterogeneous parenchyma and increased echogenicity, suggesting a chronic etiology. Given the nephrotic-range proteinuria, serologic workup for secondary causes of renal failure were sent. Workup revealed elevated light chains with a normal kappa/lambda ratio of 1.18. Urine immunofixation was unremarkable whereas the serum fixation showed weak IgG kappa and IgG lambda bands. As serological testing did not lead to a diagnosis, a renal biopsy was pursued, which revealed nodular amorphous material deposits in the glomeruli, arteriolar and arterial walls (Figure 1a) and Congo red stain showed focal apple-green birefringence (Figure 1b). There was no light chain restriction by immunofixation on pathology assessment, making AL amyloid less likely and ultimately a diagnosis of AA amyloidosis was confirmed. The patient was started on lisinopril 2.5mg daily with close outpatient nephrology and dermatology follow up initiation of immunosuppressive therapy for his HS.
Discussion: AA amyloidosis results from the deposition of amyloid fibrils derived from the acute-phase reactant serum amyloid A (SAA), which is produced in inflammatory processes. Over time, persistent inflammatory conditions like HS can lead to elevated SAA levels, which accumulate in various organs most notably the kidneys, resulting in progressive renal dysfunction. The chronic and relapsing nature of HS leads to a sustained inflammatory state, which can predispose patients to secondary systemic complications such as AA amyloidosis. In this patient, the diagnosis was suggested by the presence of nephrotic range proteinuria (3.9 g), hypoalbuminemia (2.2 g/dL), anemia, and worsening renal function, all of which are possible manifestations of renal amyloidosis but are not specific. Treatment of AA amyloidosis focuses on managing the underlying inflammatory condition to reduce SAA production.
Conclusions: This case underscores the importance of recognizing the potential for systemic complications in patients with chronic inflammatory diseases like HS. Early identification and treatment of AA amyloidosis are essential to preserve renal function and prevent further progression of renal dysfunction. Ongoing follow-up with nephrology, dermatology, and hematology is vital to monitor and manage the underlying inflammation and prevent worsening renal disease.