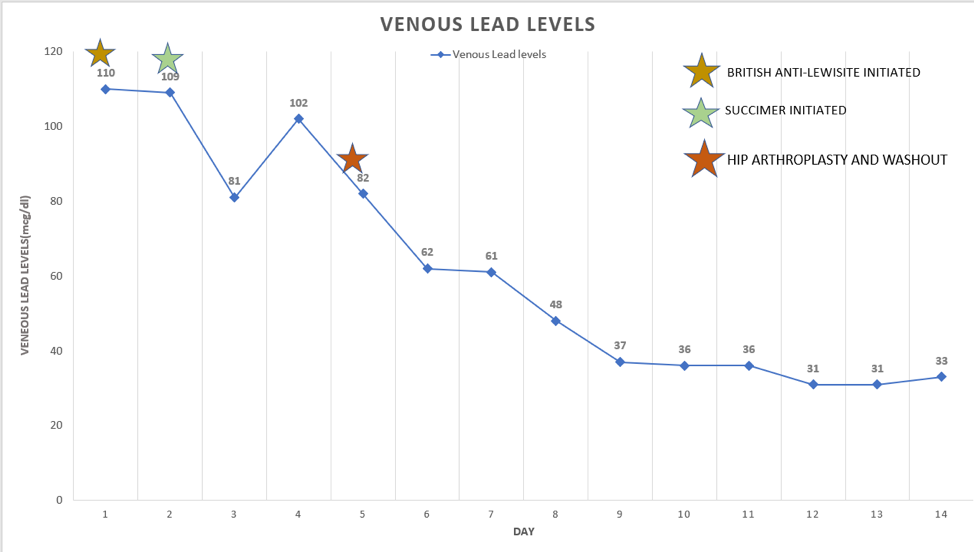
Case Presentation: A 55 year old male presented with a 1-week history of severe fatigue, constipation, and diffuse abdominal pain. He reported 1 year of progressive diffuse joint pains, numbness and tingling of bilateral upper and lower extremities, and global muscle weakness recently necessitating use of a wheelchair. He had no past medical history, and only reported a gunshot to the right hip about 32 years prior. Upon presentation, vital signs were normal. Physical exam was notable for mild diffuse abdominal tenderness. Neurologic exam revealed decreased sensation to light touch, 2/5 upper extremity strength, 3/5 lower extremity strength, and right-sided wrist drop. Lab results revealed hemoglobin of 6.7 mg/dL, low transferrin, and normal iron, TIBC and ferritin. X-ray of the right hip showed retained bullet fragments and advanced degenerative changes with marked joint space narrowing (Figure 1). Venous lead level returned elevated at 110 mcg/dL, with 24-hour urine lead level >1,000 mcg/L. Intramuscular Dimercaprol was initiated at 4mg/kg every 4 hours for 1 day, and transitioned to oral succiner 10mg/kg every 8 hours for 5 days. Washout and arthroplasty of right hip was performed for source control on hospital day 6. Venous lead steadily decreased subsequently (Figure 2). He was discharged on oral succimer and completed a 1 month course which was discontinued once blood levels were below 20 mcg/dL. However, the patient returned about 4 months later with recurrent symptoms. Repeat venous lead level was again elevated at 46 mcg/dL. Oral succimer was resumed for chronic lead toxicity due to redistribution from lead accumulation in the bones.
Discussion: The incidence of lead toxicity has dramatically decreased over the last few decades, primarily due to environmental efforts such as lead removal from gasoline and the abatement of lead-based paint (1). Adult lead poisoning today is seen mostly in occupational inhalations, however lead is still widely used in some products such as bullets (2). Soft tissue bullet wounds rarely lead to lead toxicity as these fragments tend to become encapsulated and isolated from systemic circulation (3). Although retained bullets represent less than 1% of cases of lead toxicity, unexplained and progressive neurologic symptoms in a patient with a history of gunshot wound should prompt consideration of chronic lead toxicity (4). Risk factors include advanced age, multiple bullet fragments, periarticular bone fractures, or direct contact with synovium or CSF (3,5-7). Clinical manifestations range from localized joint pain, to systemic symptoms including fatigue, constipation, neuropathy, and encephalopathy (8-10). Prompt source control and chelation therapy is critical for successful treatment (11). As in our case, it is important to note that patients may have recurrent elevations in blood lead levels after initial treatment. Lead accumulates in bone over time, and bone turnover can lead to peripheral mobilization and recurrent systemic toxicity (12,13). In these cases, treatment is long-term chelation therapy until total body lead levels are eliminated.
Conclusions: Chronic lead toxicity can be an under-recognized etiology of chronic progressive neuropathy in patients with a history of retained bullet fragments. Lead toxicity can be overlooked if physicians are unaware of the potential complications of old gunshot injuries and retained bullet fragments. A detailed history, clinical suspicion, and prompt intervention can help prevent irreversible neurologic deficits.