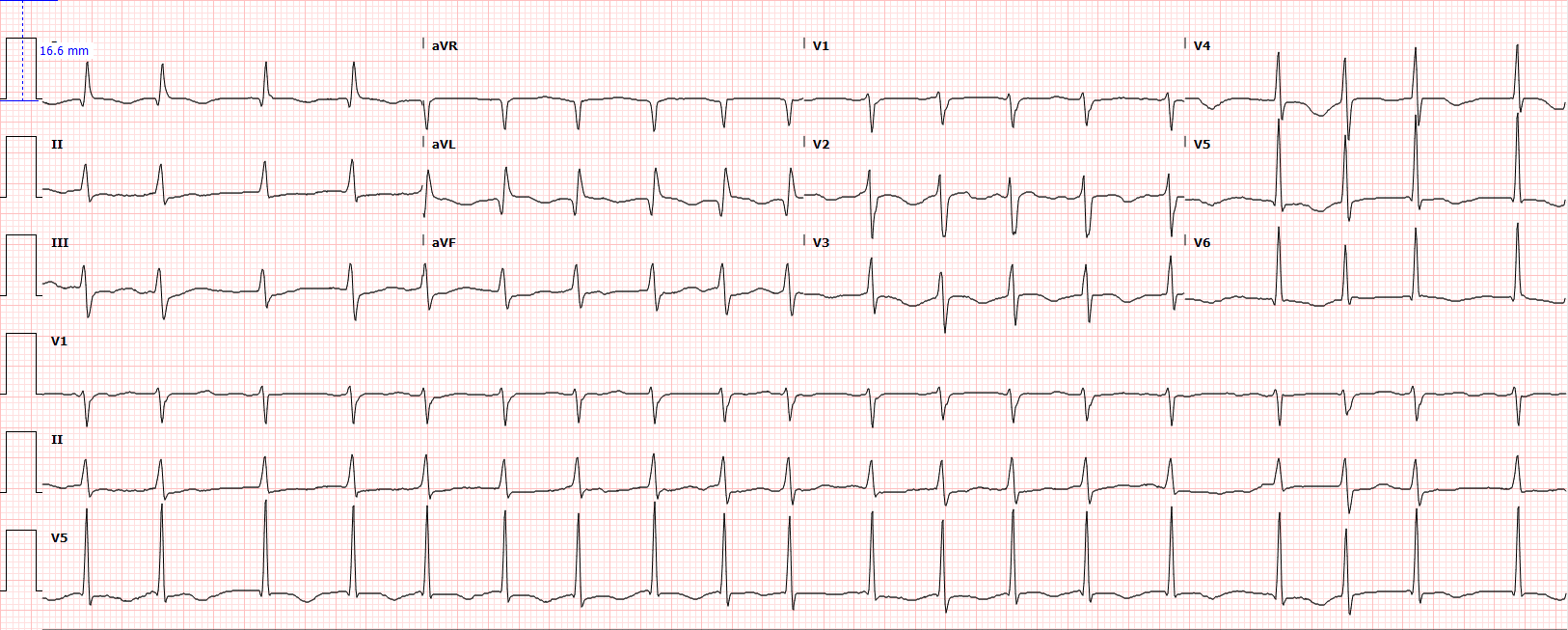
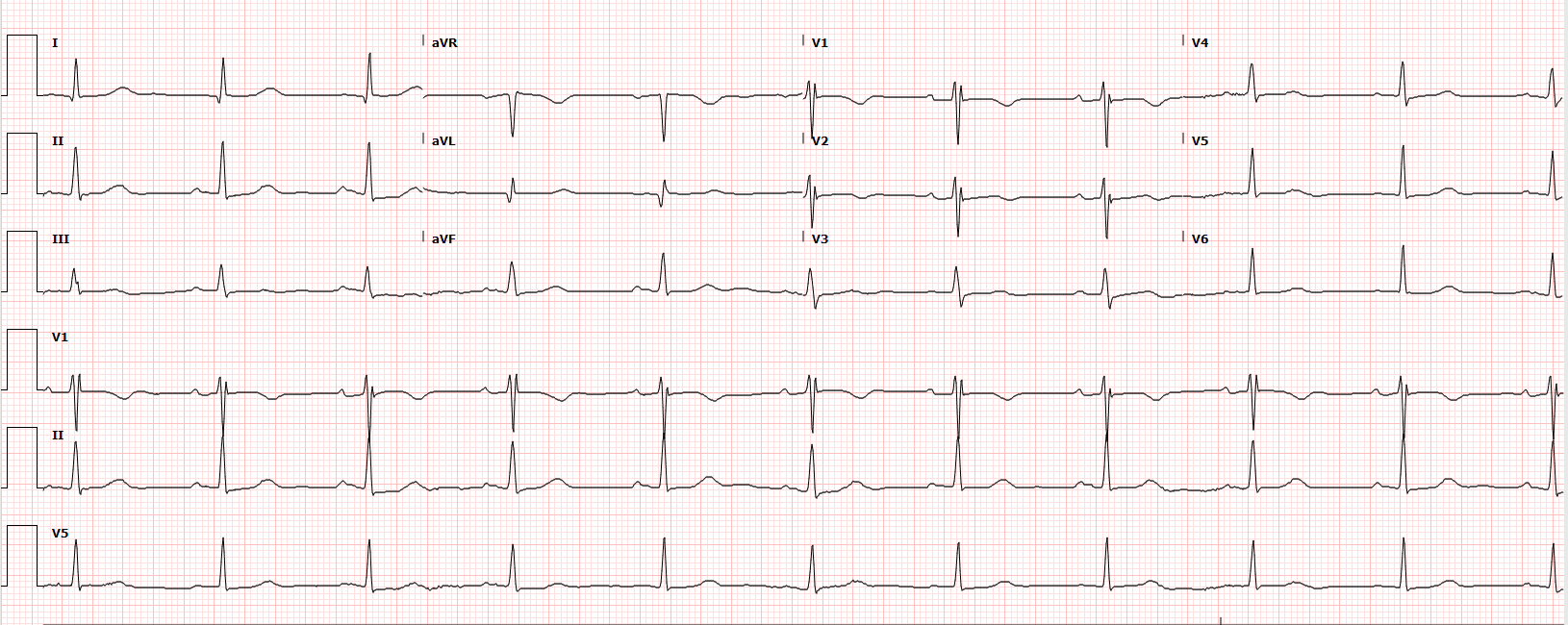
Case Presentation: 78 year old woman with persistent non valvular atrial fibrillation was admitted with palpitation and dyspnea. She was in atrial fibrillation with rapid ventricular rate. Given symptomatic atrial fibrillation after rate control, decision was made for transesophageal echocardiogram (TEE) and elective direct current cardioversion (DCCV). She was successfully converted to sinus rhythm with synchronized DC cardioversion- 200J and started on Amiodarone. However almost 48 hours after DCCV, she developed pulmonary edema and was in cardiogenic shock with lactate of 6.9. ECG showed atrial fibrillation and diffuse T wave inversion and troponin peaked at 0.73. Transthoracic echocardiogram (TTE) revealed drop in Ejection fraction(EF) to 20% from 45% few days ago and worse hypokinesis in mid-cavity compared to apex and base suggestive of mid-cavity stress induced cardiomyopathy. She was on inotropes and BiPAP with subsequent improvement and was discharged on Amiodarone, Anticoagulants and guideline directed medical therapy for heart failure with plan for ischemic evaluation as outpatient. One month later, she was symptomatically better and TTE showed recovery of EF to 55% confirming Takotsubo cardiomyopathy post cardioversion.
Discussion: Sudden LV failure leading to cardiogenic shock post cardioversion, suggestive TTE findings and complete recovery with supportive treatment support the diagnosis of Takotsubo cardiomyopathy ( TCM) post DCCV. There is a growing body of evidence behind TCM as a sequelae of DCCV and proposed mechanisms include sudden catecholamine surge mediated myocardial stunning. However, for what amount of time should the occurrence be suspected and patients be warned about the symptoms is still not clear. This is important especially when patients are discharged home on same day after DCCV. There are reports on TCM on immediate phase after DCCV and up to 10 hours later, but our patient presented 48 hours later and had a complicated course. Although it is a completely reversible condition, immediate prognosis is grave if not identified and treatment initiated in a timely manner.
Conclusions: Electrical cardioversion is a very well tolerated procedure in the management of cardiac arrhythmias. Although it has good success rates, awareness of complications is important in clinical practice. Venous thromboembolism and recurrence of arrhythmia are the commonly described complications. Here we present a case of takotsubo cardiomyopathy (TCM) resulting in cardiogenic shock, a rare but possible complication of cardioversion that happened almost 48 hours after cardioversion.