Background: The nature of the Advanced Practice Provider (APP) and attending physician (MD) relationship is that of trust, mutual respect, and delegation. In U.S. territories where MD supervision or oversight of APP practice is required by law, MDs are left to trust and delegate patient care tasks and authority to their collaborating APPs while sharing medical liability. While effective collaborating relationships are of great importance for MD/APP hospitalist teams, there are few guidelines or evidence supporting ideal collaborative care. At our hospital, we undertook a process to better understand the ideal levels of autonomy and collaboration on MD/APP hospitalist teams across various domains of care.
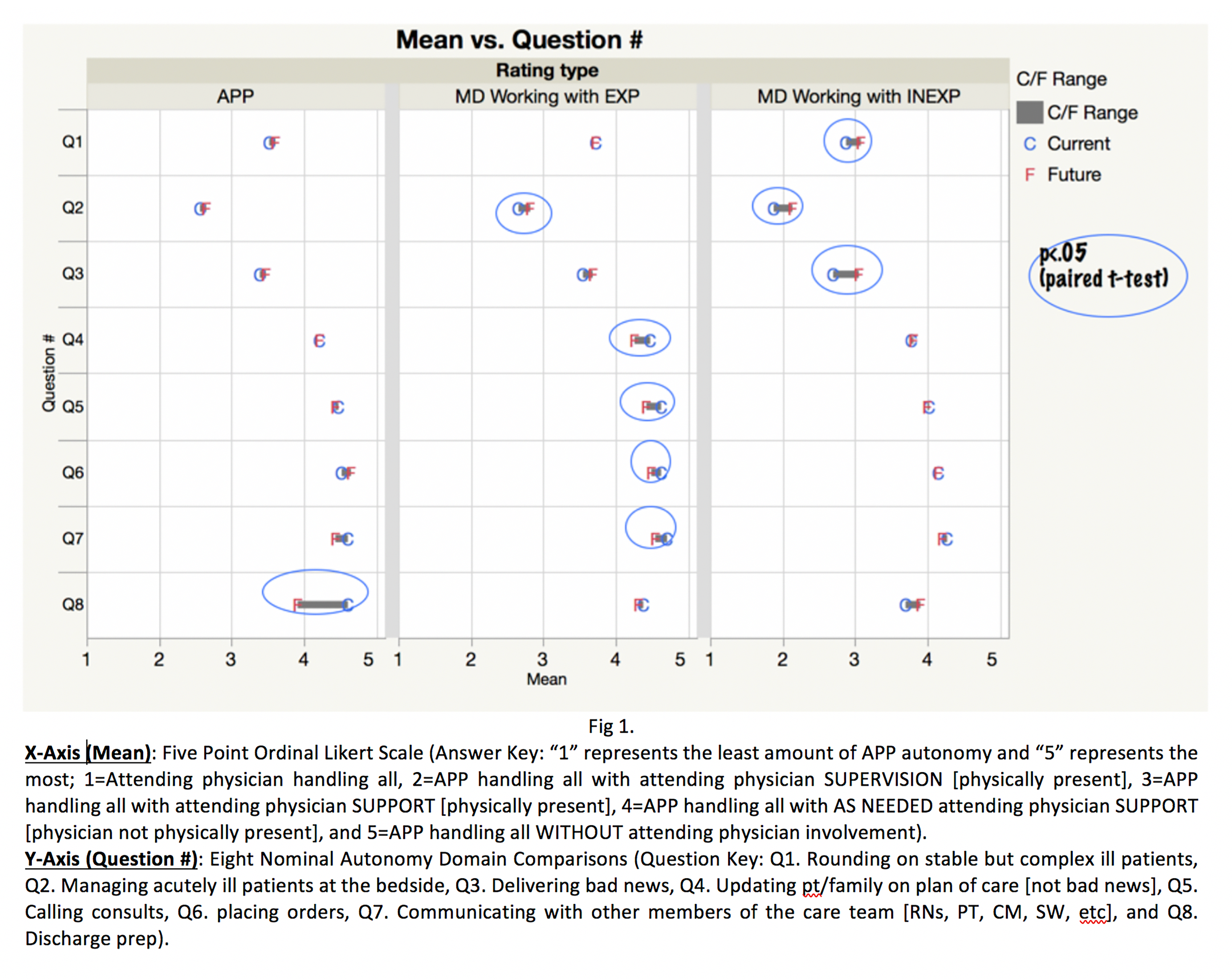
Methods: We assembled multiple focus groups from within the Massachusetts General Hospital Hospital Medicine Unit (HMU) and, via a modified Delphi process, created surveys for both APPs and MDs. Surveys focused on eight key task-related domains built around the core ideals of communication, documentation, and clinical decision making. The surveys captured respondent level of experience as well as their view of the current state and their ideal state for collaborative practices between APPs and attending physicians. Respondents were also given the opportunity to leave free-text comments to identify trends not otherwise addressed in the task-related domains. For the eight identified domains, t-tests were performed measuring the differences between APP and attending physician responses on a five-point ordinal Likert scale: 1=Attending physician handling all, 2=APP handling all with attending physician SUPERVISION (physically present), 3=APP handling all with attending physician SUPPORT (physically present), 4=APP handling all with AS NEEDED attending physician SUPPORT (physician not physically present), and 5=APP handling all WITHOUT attending physician involvement.
Results: 76 MDs and 23 APPs responded to the surveys, representing 70% of all staff. Overall, there was general agreement between MDs and experienced APPs in the desired level of autonomy across all 8 domains other than discharge preparation, in which experienced APPs felt that they would like more support in an ideal future state. MDs felt that when working with inexperienced APPs, they wished for less supervisory responsibility in the future across the domains of rounding on stable but complex or ill patients, managing acutely ill patients, and delivering bad news. In free-text comments, both APPs and MDs also identified the need for attending physician presence when caring for acutely ill patients, as well as needing 360-degree feedback and the importance of closed loop communication.
Conclusions: Currently, there are minimal published guidelines to suggest what teamwork dynamics around autonomy lead to optimal collaborative care. At our institution, we utilized a modified delphi process and staff surveys to arrive at consensus about desired autonomy across 8 practice task-related domains. Our results demonstrate that MDs and APPs are generally aligned, favoring more physical presence of MDs when providing support for inexperienced APPs and across domains that are higher-risk for patients, such as acute decompensations requiring bedside management. These results can serve as a roadmap to establishing autonomy expectations for MD/APP collaborative care teams at our hospital, and might have utility in other hospitals or care settings.