Background: Hospital readmissions among HIV positive patients are high, and reducing 30-day readmissions is a priority of health systems and payers. Improved communication in the hospital may help decrease readmissions. Our objective was to determine the association between satisfaction with provider communication and 30-day readmissions among HIV positive patients.
Methods: We performed a cross-sectional analysis of patients with HIV (captured with ICD9 codes 042 and V08) admitted to Johns Hopkins and affiliated hospitals, from January 2008 to March 2015. Data pertinent to hospital admissions was obtained from Casemix Datamart whereas patient satisfaction variables were abstracted from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey responses. HCAHPS communication scores were adjusted to derive the independent variable which was dichotomized into “High satisfaction” or “Suboptimal satisfaction” for both doctor and nurse communication. The outcome variable was the occurrence of 30-day readmission. Logistic regression was performed to determine the association between 1) doctor communication satisfaction 2) nursing communication satisfaction and 3) instructions regarding warning symptoms at discharge and 30-day readmission. Regression models were adjusted for age, sex, race, length of stay, number of chronic medical conditions and whether or not the patient was admitted to Infectious Disease Service.
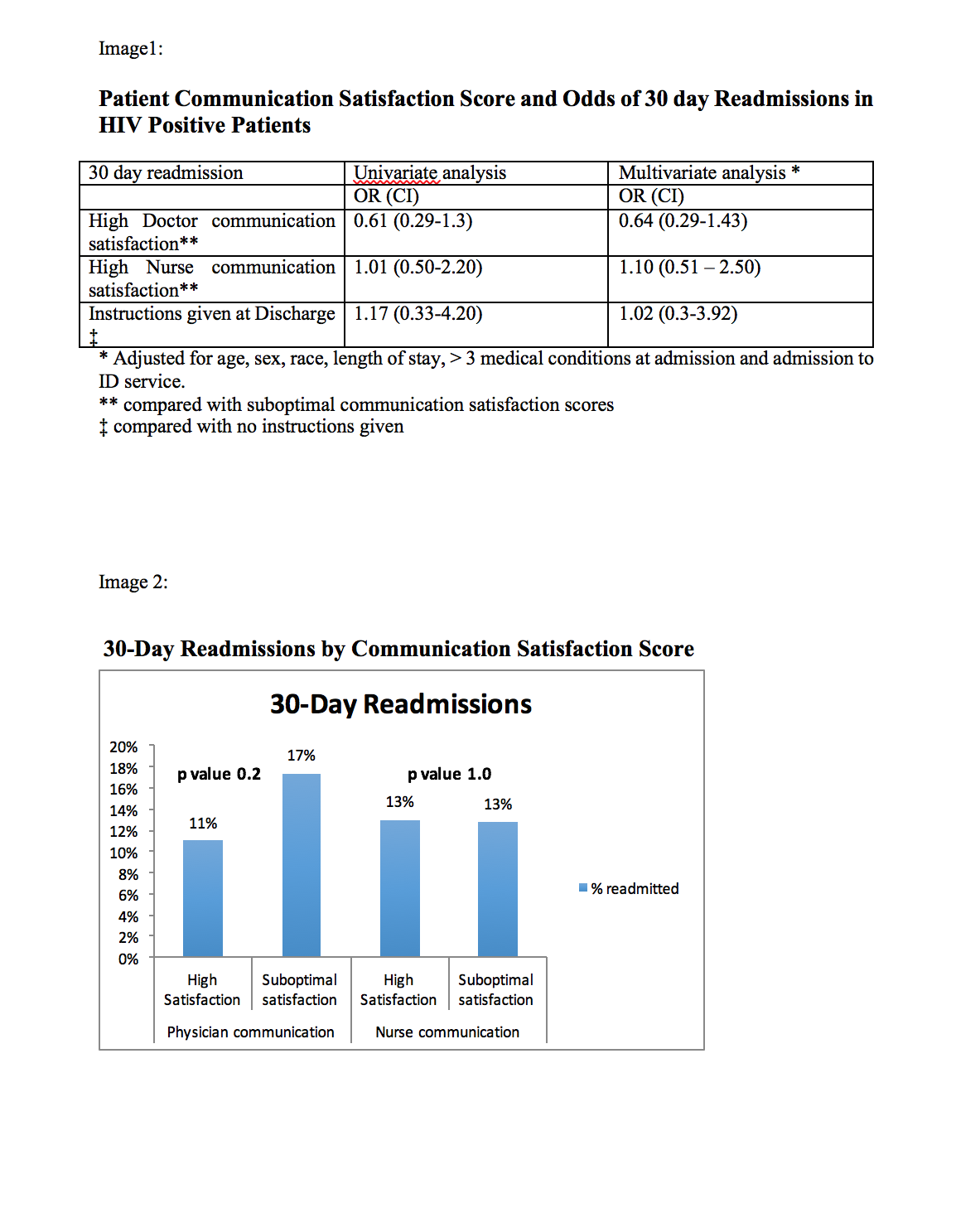
Results: 1416 HIV positive patients received the survey (55% men, 78% African American, 75% with Medicare/Medicaid, mean age 46 years). Mean length of stay was 3.2 days. About 15% of HIV positive patients were readmitted. Male sex (OR 1.3, 95% CI 0.5 – 0.9, p=0.03), longer hospital stay (OR 1.12, 95% CI 1.1-1.2, p < 0.001), and having 3 or more chronic conditions (OR 1.52, 95% CI 1.1-2.0, p 0.007), and admission to the ID service (OR 1.37, 95% CI 1.0 – 1.8, p 0.03) were associated with 30-day readmission. 75% of HIV-positive patients were highly satisfied with physician and 70% were highly satisfied with nursing communication. In univariate and multivariate analysis, there was no difference in the odds of 30-day readmission comparing patients highly satisfied with doctor communication to those with suboptimal satisfaction (OR for MV analysis 0.64, 95% CI 0.3-1.4). Similar results were found for satisfaction with nursing communication (OR comparing high satisfaction to suboptimal satisfaction = 1.2, 95% CI 0.60, 2.50).
Conclusions: A high proportion of HIV–positive patients report high satisfaction with provider communication during hospitalization although it was not associated with 30-day readmission. Effective communication during hospitalization can be an opportunity to identify and address barriers to health care which could potentially reduce 30-day readmissions in this marginalized population.