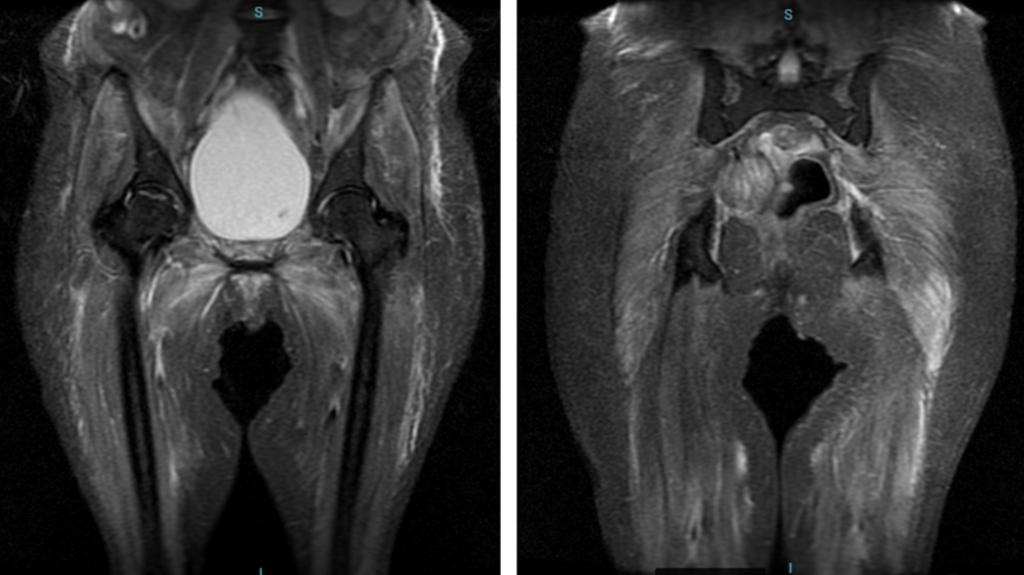
Case Presentation: A 48-year-old woman with a history of fibromyalgia presented with a three-month history of progressive dyspnea, muscle weakness, weight loss (20 kg), and worsening respiratory symptoms. She initially sought care for productive cough, fever, and dyspnea, receiving treatment for pneumonia with ceftriaxone on two occasions with transient symptom relief. However, her symptoms recurred alongside pruritic skin eruptions (Figure 1), culminating in referral to a tertiary care hospital.On admission, she was pale, tachypneic at rest, and required supplemental oxygen. Physical exam revealed capillary rarefaction, oral ulcers, arthralgia, and progressive muscular weakness, impairing her ability to perform daily activities. Laboratory findings showed normocytic normochromic anemia, elevated inflammatory markers (ESR 84 mm/h), and complement consumption (low C3 and C4). Autoimmune workup identified antinuclear antibody (ANA) 1:640 (homogeneous), anti-Ro positivity, and low anti-DNA titers (1:40), but anti-RNP negativity.Imaging demonstrated bilateral pleural effusions, pericardial effusion, axillary and retroperitoneal lymphadenopathy, and mesenteric fat nodules. CT angiography excluded pulmonary embolism. During hospitalization, the patient developed acute respiratory failure requiring intubation but was successfully extubated after four days. MRI confirmed significant muscular edema in the pelvic (Figure 2) and scapular girdles and muscular atrophy. Electromyography revealed a myopathic pattern in the right deltoid, biceps, and vastus lateralis.Systemic lupus erythematosus (SLE) was diagnosed, and treatment with hydroxychloroquine (400 mg/day) and prednisone (40 mg/day) was initiated. Subsequent findings of myositis prompted therapy with high-dose methylprednisolone (500 mg/day for three days) and intravenous immunoglobulin (2 g/kg). The patient showed marked improvement, regaining ambulation with assistance and discontinuing supplemental oxygen at discharge. She continues outpatient treatment with methotrexate, hydroxychloroquine, and scheduled immunoglobulin infusions, with tapering corticosteroids and sustained clinical improvement.
Discussion: Overlap syndrome refers to the simultaneous presence of clinical and immunological features of two or more connective tissue diseases in a single patient. The co-occurrence of SLE and myositis is rare, predominantly affecting women, and may portend a worse prognosis. This case underscores the importance of recognizing overlap syndromes as a differential diagnosis in patients with systemic autoimmune manifestations, particularly when respiratory failure and muscular involvement are noted. Timely diagnosis and immunomodulatory therapy can dramatically alter the disease trajectory, preventing complications and improving quality of life.
Conclusions: SLE-myositis overlap syndrome is a rare but potentially severe condition. Early diagnosis and tailored treatment are essential to achieving favorable outcomes. This case highlights the importance of prompt immunomodulatory therapy in managing respiratory failure and muscular weakness associated with overlap syndrome. Hospitalists play a critical role in the diagnostic and therapeutic approach, emphasizing the necessity of recognizing complex connective tissue disease presentations, collaborating closely with Rheumatology through consultation, and ensuring safe discharge with a smooth transition to the outpatient setting.