Background: Nocturnists often start their positions immediately after residency. It has been shown that early career hospitalists benefit from mentorship for scholarly productivity, academic promotion and personal career satisfaction (1,2). However, as nocturnists typically work at different hours than senior clinicians and service leaders, there are decreased opportunities for informal mentorship, modelling, and visibility.
Purpose: An early career nocturnist mentorship program was designed to help nocturnists identify an area of career focus, find a mentor, and promote career success.
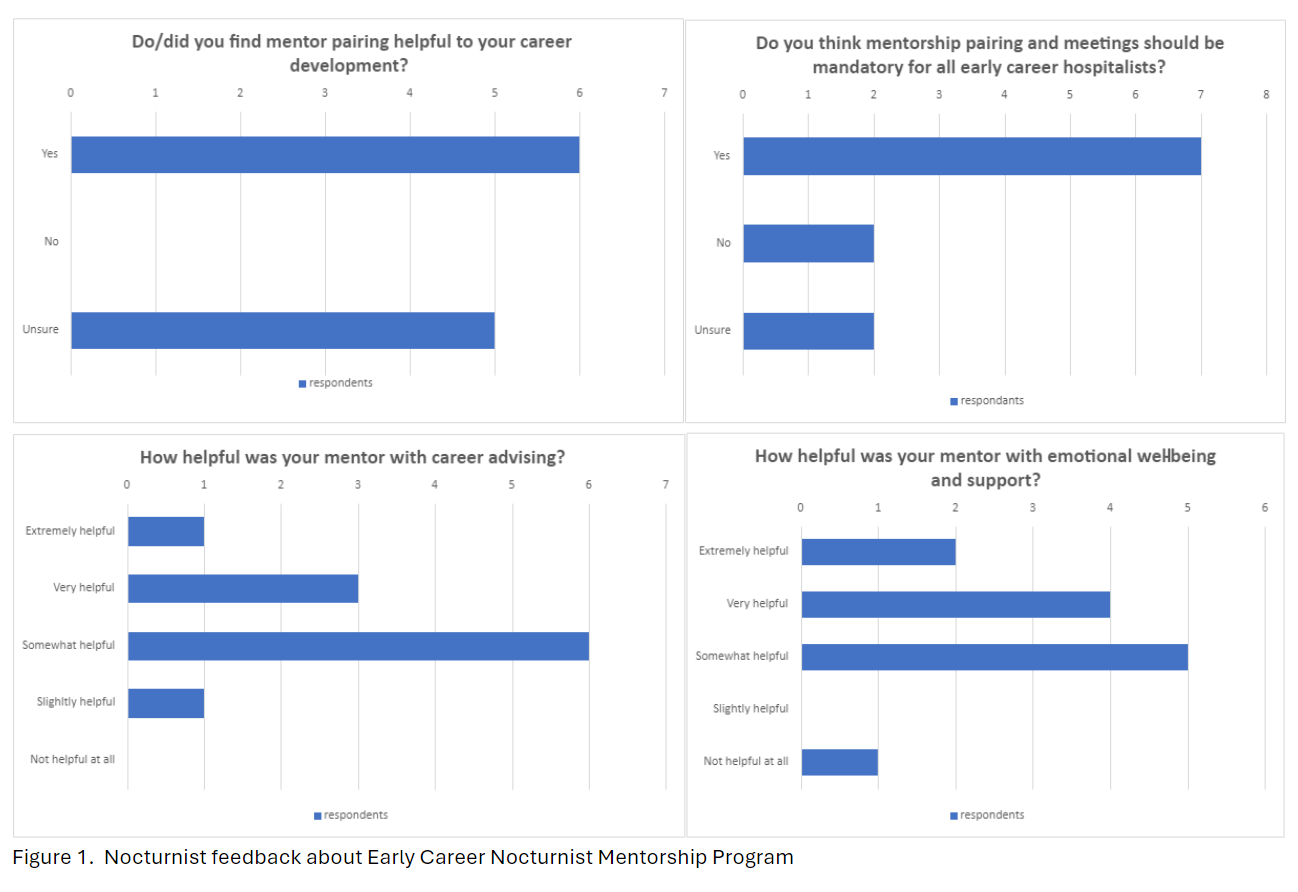
Description: In 2021, an Early Career Nocturnist Mentorship program was created at an academic hospital with 25 nocturnists. Every new nocturnist who intends to stay in the role for more than 1 year is invited to join. Participants have an initial meeting with the Mentorship Program and Nocturnist service leaders. They explore the nocturnist’s interests and goals, focusing on medical education, patient care processes, research, and other areas of expertise (3). The leaders identify mentors from within the institution who may be senior hospitalists (day or night) or clinicians outside of hospital medicine with similar interests. These potential mentors are then invited to participate. Introductions are made, with a description of shared interests and the purpose of the program. The nocturnist/mentor pair determines the frequency of meetings. The leaders then conduct check-in meetings to assess the pairing and progress toward goals. An 18-item survey was sent to all 16 nocturnists in the program through 2023, to obtain anonymous feedback about the program and mentors. 11 surveys were completed (69%). 91% felt their mentor was aligned with their clinical interests. The pairs met with frequency ranging from monthly to biannually. Nocturnists were asked how helpful their mentors were with attaining their goals using a Likert-type scale. For nocturnists interested in teaching, quality improvement (QI), research, and committee work, mentors were very or extremely helpful to nocturnists 42%, 100%, 100%, and 66% of the time, respectively. More broadly, 30% of nocturnists found their mentors helpful with clinical skills support, 40% with career advising, and 60% with emotional well-being and support. While 45% were unsure if their mentorship pairing was helpful in their career development, 64% felt that mentorship pairing and meetings should be mandatory for all early career hospitalists. As a result of this program, leaders have noted that early career nocturnists have been able to find teaching opportunities at the medical school, participate in various hospital committees, develop curriculum for trainees and faculty, and design and implement QI/research projects. Since implementation of this program, 4 nocturnists have been promoted. Internal letters in support of nocturnist academic promotion have been obtained from multiple mentors in this program.
Conclusions: This is the first reported mentorship program specifically designed for nocturnists, with successful results for many participants. Mentorship for nocturnists needs to be intentional and flexible to balance the need for sleep during the day with the desire to grow a career, even while working at night. To retain nocturnists, and ensure that nocturnist work does not create career stagnation, hospitalist service leaders should put intentional effort into mentorship of early career nocturnists, who may be less visible due to their night schedule.