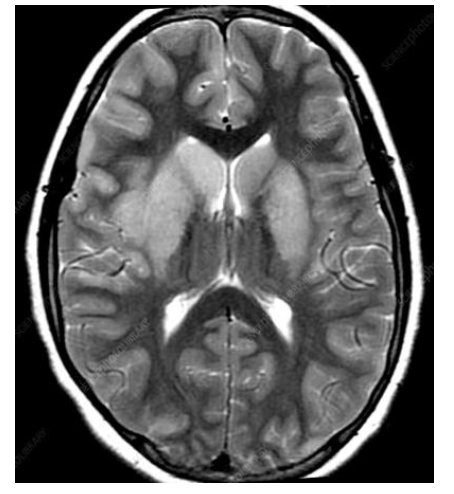
Case Presentation: A female patient in her 70s, with a history notable for hypothyroidism who initially presented to an outside hospital with complaints of left-hand paresthesia, numbness, and dizziness. She underwent an extensive work up for CVA with no acute findings on non-contrast MRI brain or cervical spine. During her hospital course she developed worsening encephalopathy, and rapidly progressing quadriparesis, the patient was treated with a 5-day course of IVIG, for a concern of Guillain-Bare syndrome (GBS). However, CSF findings were notably inconsistent with GBS. Her symptoms were presumed to be due to a viral etiology in the setting of pleocytosis seen on CSF. Due to a high risk of decompensation, the patient was transferred to a higher level of care, where she underwent repeat MRI imaging with and without contrast of the brain and spine, as well as a repeat lumbar puncture for additional CSF studies. She was started on empiric Acyclovir, Ceftriaxone and Doxycycline for possible HSV and tick- borne infection, respectively. She also received a trial of pulse dose steroids with significant clinical improvement. Although, most of her workup returned negative, her EBV PCR was positive, confirming EBV encephalitis. Given the patients’ significant clinical improvement of encephalopathy and paresis on steroids, she was transitioned to a prednisone taper and discharged to rehab with a follow up with neurology and infectious disease.
Discussion: Epstein-Barr Virus (EBV) has been reported to cause around 5% of all viral encephalitis cases [2]. The exact pathogenesis of EBV is unclear, but direct viral invasions and autoimmune response directed against the brain is believed to cause symptoms and imaging findings. Currently, there are no guidelines for the treatment of EBV encephalitis, and the standard of care is supportive treatment. The effectiveness of treatment with acyclovir and steroids remains unclear, however early treatment is recommended in critically ill patients whose prognosis is uncertain. As evidenced in our case, this approach certainly can be utilized, as it improved symptoms for our patient. Given the complexity of diagnosis and treatment, EBV should be considered as a possibility in all acute encephalopathic presentations, with diagnostic testing.
Conclusions: Epstein-Barr Virus (EBV) is a well-known pathogen that is associated with infectious mononucleosis. However, EBV although rarely, can present with neurological manifestations. EBV encephalitis is not commonly seen in immunocompetent adults and has been associated with immunocompromised patients. This includes those with hematopoietic stem cell transplants, solid organ transplants, and HIV infections. Most reported cases of EBV encephalitis were observed in children, and little is known about its presentation in an adult. We discuss a case of EBV encephalitis that highlights its complex clinical manifestation that makes it a difficult diagnosis.