Background: Up to 18% of clinic patients are considered difficult by their providers. (1,2) Common characteristics of difficult outpatients are the presence of personality disorders, depression, anxiety, somatization and requesting pain medications. (1,2, 5) Two qualitative studies suggest that inpatient medicine providers also regularly experience hospitalized patients as difficult. (3,4) However, there have been no studies of medicine inpatients that have estimated the prevalence and characteristics of difficulty.
Methods: Inpatients were randomly selected and their inpatient providers (hospitalists, non-hospitalist medicine faculty, medicine residents and interns) completed online surveys rating patient difficulty on dichotomous (yes/no) and continuous (0-10) scales. Characteristics abstracted from the chart included patient demographics, cognitive status, Charlson comorbidity index, length of stay, and whether the patient had a chart diagnosis of depression, anxiety, PTSD, chronic pain, somatization disorders or personality disorders. In addition to descriptive statistics, generalized linear latent and mixed models with random intercepts for number of evaluations was used to investigate patient and provider characteristics associated with difficulty. Kappa was used to assess inter rater agreement.
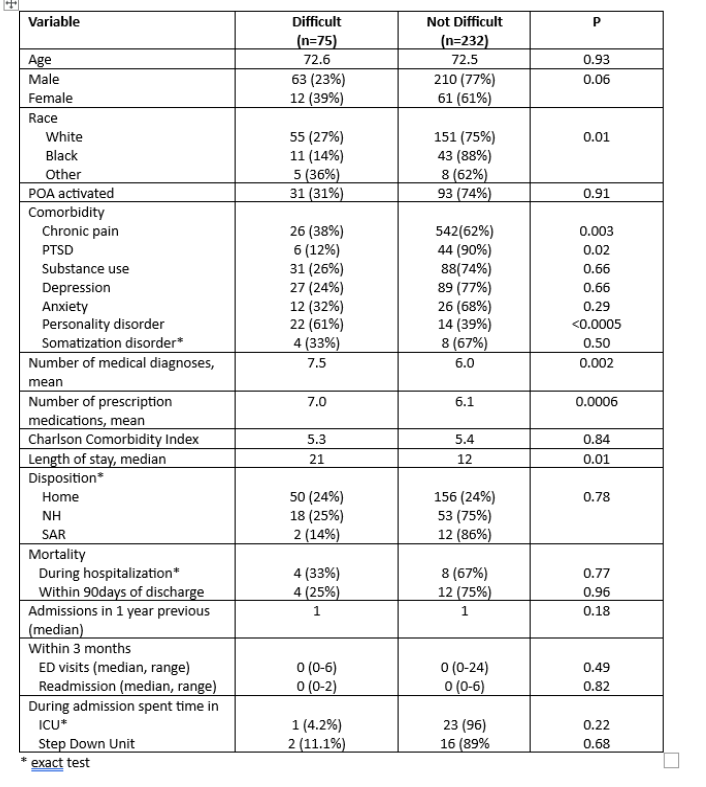
Results: Two hundred and seventy-nine patients were randomly selected with 307 surveys submitted; at least one survey was completed for 192 patients (69% response rate). One hundred and nine patients were rated once. The remaining patients were rated more than once by unique providers: 63 by two, 12 three times, 5 four times, 2 five times and 1 patient by 6 different providers. The patients’ average age was 72.5 years (range 30-102), 91% were male, 70% were white and 27% black; 69% were discharged to home. The median length of stay was 12 days (range 1 to 373) and 26% were readmitted within 90 days of discharge. The average Charlson Comorbidity Index score was 5.3. Chronic pain was present in 20% (n=37) of inpatients; 17% had PTSD, 39% had depression and 13% had anxiety. Five percent of patients died during hospitalization and another 6% died within the first 90 days after discharge.Overall, 24.5% of medicine inpatients were considered difficult. There was no difference in average difficulty score between rater types (hospitalists, non-hospitalist medicine faculty, residents or interns, p=0.36). Respondents had modest agreement on patient difficulty (k=0.33). Gender, race, length of stay, number of medications and comorbidities, personality disorders and chronic pain were associated with being considered more difficult on univariate screen (Table 1). However, only personality disorders (OR: 5.4, 95% CI: 2.9-10.3) and chronic pain (OR: 2.0, 95% CI: 1.1-3.6) independently increased the likelihood of difficulty on multivariate assessment.
Conclusions: .Medicine inpatients are commonly experienced as difficult. The prevalence appears to be higher in hospitalized than clinic patients. Chronic pain and personality disorders increased the likelihood of being experienced as difficult. Some characteristics common among difficult clinic patients (depression, anxiety, somatization) did not increase inpatient difficulty.These results need to be validated in a non-VA population and could inform future work with managing physician perceptions/interactions with difficult inpatients.