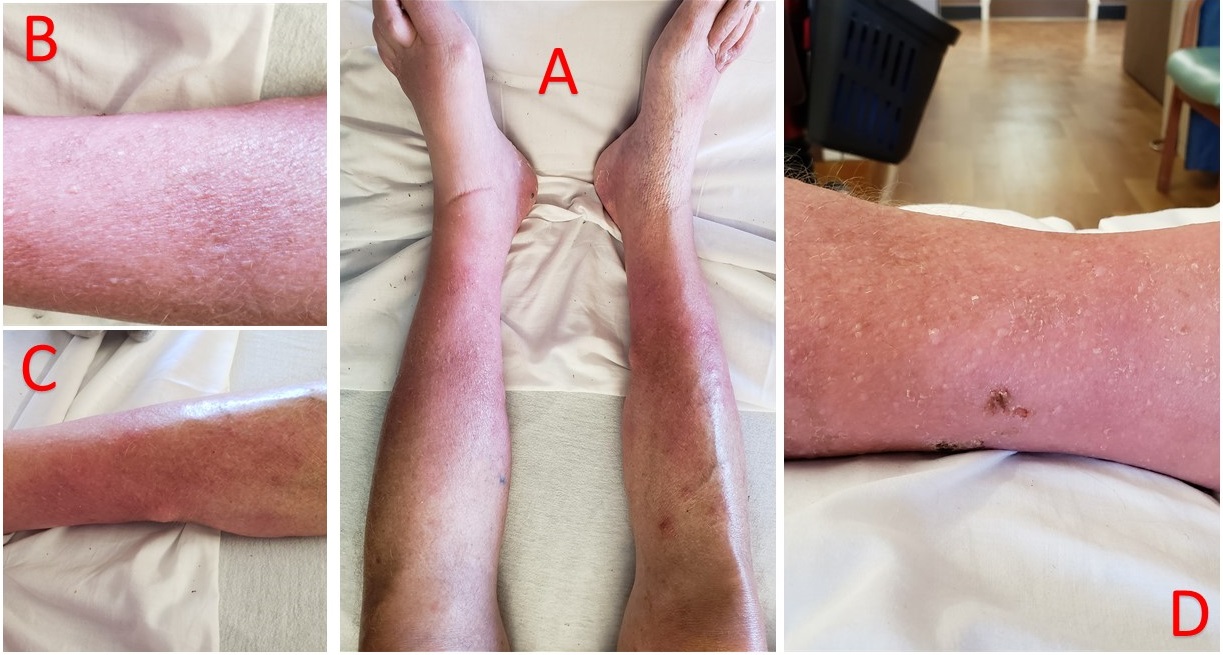
Case Presentation: A 65-year-old man with a past medical history of gout and chronic pancreatitis complicated by pseudocyst presented with bilateral lower leg swelling, erythema, and pain for few weeks. The rash was also associated with bilateral lower extremity nodules that would spontaneously open and discharge white material. He was seen and treated in the outpatient setting with multiple courses of oral antibiotics with minimal improvement. The patient was hemodynamically stable, his physical exam was significant for erythema, warmth, exquisite tenderness and edema to his both lower extremities extending from feet to mid-calves with multiple nodules, measuring approximately 3 cm in diameter, and with faint peripheral pulses. He was started on IV vancomycin treatment to treat possible refractory cellulitis, his symptoms of erythema, warmth and tenderness had improved and the patient was discharged home with doxycycline and cephalexin to complete a prolonged course of antibiotics. Five days after discharge, he returned with recurrent erythema, warmth and severe pain in his bilateral lower extremities. His physical exam was similar to his prior presentation. A CT angiogram of the lower extremities was performed which including the aortic origin and revealed severe arterial disease and an incidental finding of an enlarging pancreatic mass, presumed to be pancreatic pseudocyst. The mass was further confirmed by pancreatic MRI which revealed interim growth of the pancreatic mass with stable pancreatic duct dilatation. Lipase and amylase were elevated to >4200 U/L and >2100 U/L, respectively. Skin biopsy was obtained, which exhibited ghost cells and saponification within the subcutaneous tissue, consistent with pancreatic panniculitis.
Discussion: Pancreatic panniculitis is rare with an estimated incidence of 2-3% in pancreatic disease, with about 45% of the patients have an underlying malignancy. The cause of the disorder is unknown, but a role for the release of pancreatic enzymes has been proposed giving the high level of lipase and amylase seen in these patients. Diagnosis is made through clinical features of rash which mostly involves distal extremities in addition to skin nodules that may ulcerate and drain oily brown liquid derived from the necrosis of adipocytes, clinical diagnosis should be paired with skin biopsy results showing primarily lobular panniculitis with extensive necrosis of adipocytes and ghost adipocytes (adipocytes without nuclei) with calcium deposits. Treatment should involve treating the underlying cause and relieving of any obstruction in the pancreatic duct if present. However, in patients with pancreatic carcinoma, the course of panniculitis tends to be more persistent.
Conclusions: In patients presenting with what appears to be bilateral lower extremity cellulitis, clinical suspicion should be raised to expand the differential diagnosis. Hospitalists should consider pancreatic panniculitis as a potential diagnosis in patients with chronic pancreatitis presenting with rash and subcutaneous nodules.