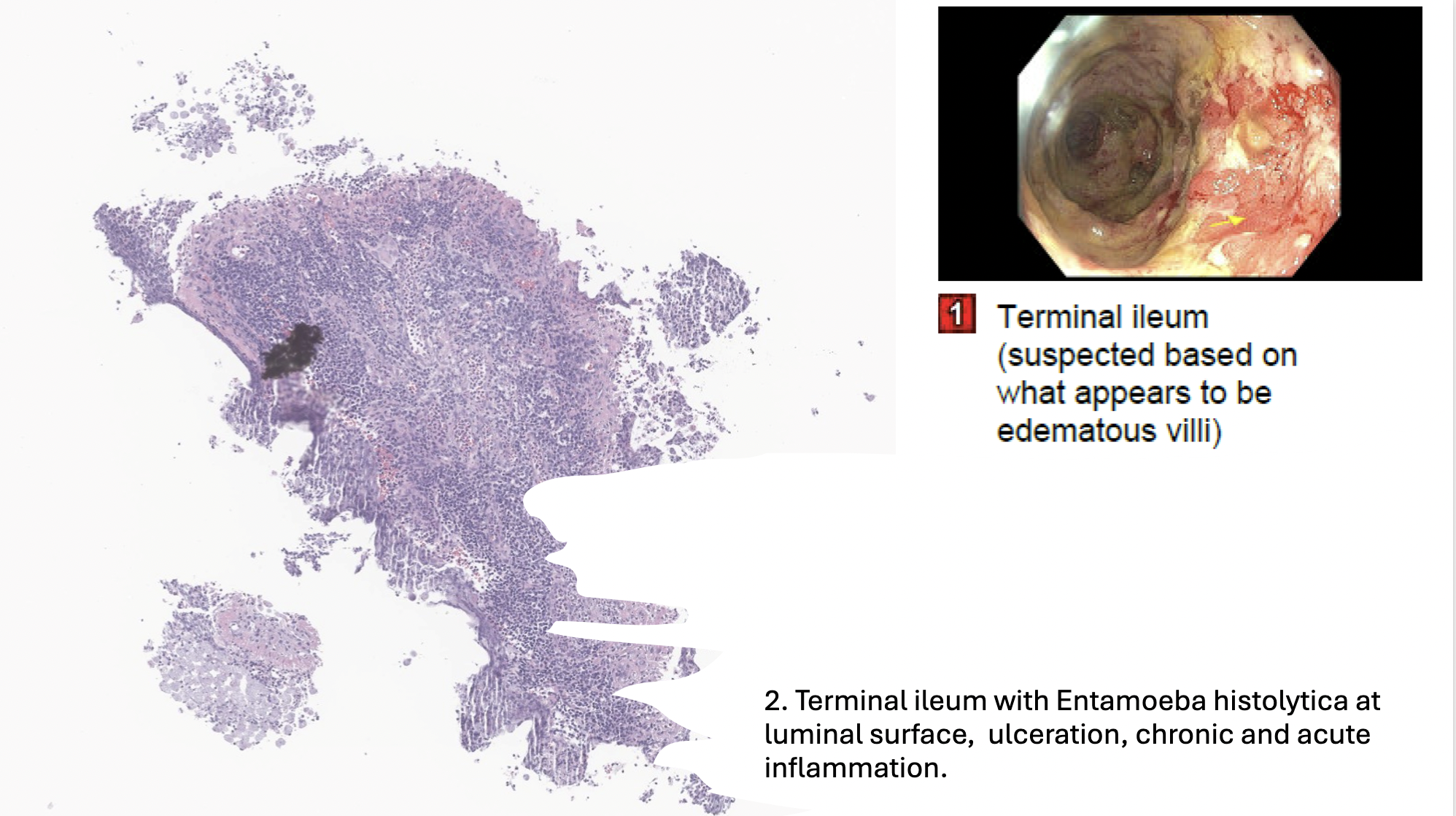
Case Presentation: A 56-year-old M was admitted in Rhode Island with abdominal pain, malaise, and copious loose, bloody stools for 9 days after recurrent ED and outpatient visits for the same symptoms. His diarrhea had worsened despite outpatient amoxicillin-clavulanate, and he was sent back to the ED by GI due to hyponatremia (Na 129) and hypokalemia (K+ 2.7). CT showed wall thickening of the cecum, ascending colon and transverse colon with dilation and fluid-filled segments. Recent ED work-up was notable for mild leukocytosis at 12.6K, negative stool pathogen PCR (salmonella, shigella, campylobacter, vibrio, Y. enterocolitica, norovirus, rotavirus) and C difficile, negative cryptosporidium and giardia, and CRP of 20.7 with normal lactate. Additionally, lipase, cytomegalovirus, anaplasma, ehrlichia, babesia, Lyme, immunoglobulin A, QuantiFERON gold and hepatitis panel returned normal. GI was consulted and performed colonoscopy showing diffuse, severe intestinal inflammation with erosions, erythema, friability, and deep ulcerations in the entire colon and into the terminal ileum. Pathology showed early but severe, moderate chronic colitis in a patchy distribution. No microorganisms, granulomata, viral cytopathic effects, basal lympho-plasmacytosis or vasculitis were identified. He was treated with IV ceftriaxone and metronidazole for 2 days. Given his clinical picture and pathology results favoring inflammatory bowel disease (IBD), IV methylprednisolone was initiated. He was discharged on a prednisone taper with GI follow-up. He was readmitted 2 weeks later with recurrent loose stools and abdominal pain that were attributed to dose reduction in prednisone from 40mg to 30mg. He was restarted on IV steroids with improvement in CRP but had persistent maroon stools. He was discharged with a plan for outpatient infliximab 5mg/kg which he received the next day. His symptoms of bloody diarrhea then worsened and given his 26lb weight loss over the last month, he presented to Yale New Haven Hospital. Outside hospital records, imaging, and pathology results were reviewed and deemed consistent with steroid-dependent Crohn’s ileocolitis. He was restarted on IV steroids and received 2 doses of infliximab 10mg/kg. CRP decreased from 183 to 16.5, though symptoms only minimally improved. He then underwent repeat colonoscopy that showed large ulcerations with friable mucosa throughout the colon and terminal ileum (>75% surfaces affected). Pathology returned with diffuse intraluminal amebiasis and inflammation. The patient had no recent travel outside of the northeastern US. He was started on IV metronidazole and stool O+P microscopy was sent, which resulted positive for both Entamoeba coli and Entamoeba histolytica 10 days later. He was transitioned to paromomycin on discharge. His symptoms continued to resolve over the following 2 weeks.
Discussion: E. histolytica is common to resource-limited countries worldwide but is not endemic to New England. It is most often asymptomatic but can cause severe disease with fulminant colitis, dysentery, and hematochezia. Patients who receive steroids due to initial misdiagnosis can have rapid disease progression with up to 25% mortality. PCR or antigen testing are preferred due to higher sensitivity and quicker results compared to stool microscopy.
Conclusions: In patients with a new diagnosis of possible IBD that does not respond to typical treatment, E. histolytica and other pathogens should be considered to prevent misdiagnosis and worsening of infectious diarrhea.