Background: A lack of standardization in care delivery can lead to variations in outcomes in the high-risk work of neurosurgery. The aim of this program was to develop, implement and evaluate the impact of three standardized interventions to improve neurosurgical patient outcomes and experiences.
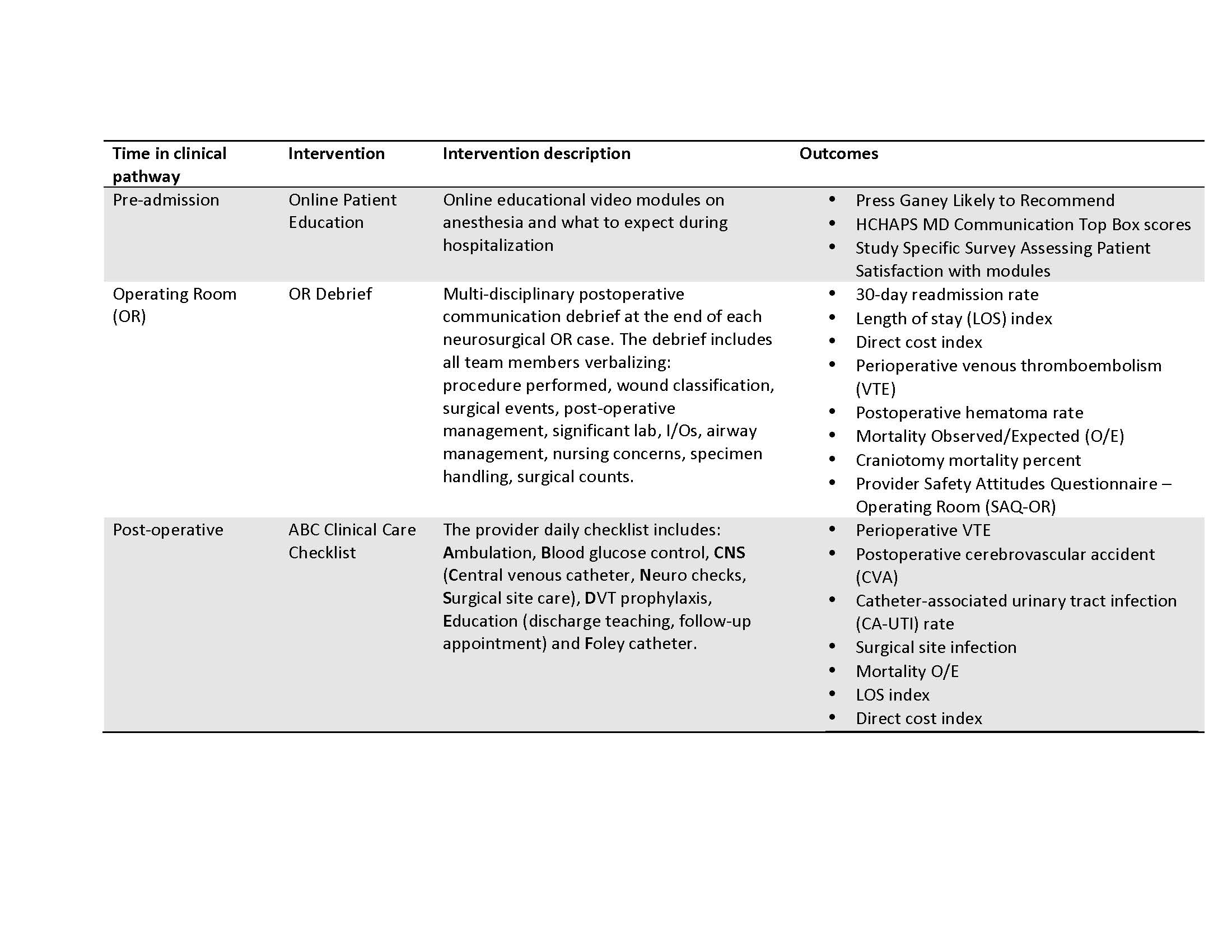
Methods: Hospitalists partnered with Anesthesia and Neurosurgery leaders from five large urban academic medical centers to form a quality improvement collaborative. We developed three evidence-based interventions to standardize specific pre-admission, operative and post-operative processes (Table 1). All adult patients (≥18 years) admitted for an elective or emergent neurosurgical procedure were eligible. We used a prospective interrupted time series study design to assess trends in patient clinical and satisfaction outcomes during the pre-intervention (04/01/12-03/31/14) and post-intervention (04/01/14- 03/31/16) time periods (Table 1).
Results: There were 11,447 neurosurgical patients in the pre-intervention and 10,973 in the post-intervention period. We successfully prescribed 15,965 pre-admission online education modules with prescription rates higher than 84% at all centers. Patients’ 90-day module viewing completion rates vary by site (20 to 45%). We implemented a multi-disciplinary operating room debrief at the end of each neurosurgical case – debrief compliance varies by site (41-100%). All sites have integrated the ABC Checklist into their electronic health record through the daily progress note.
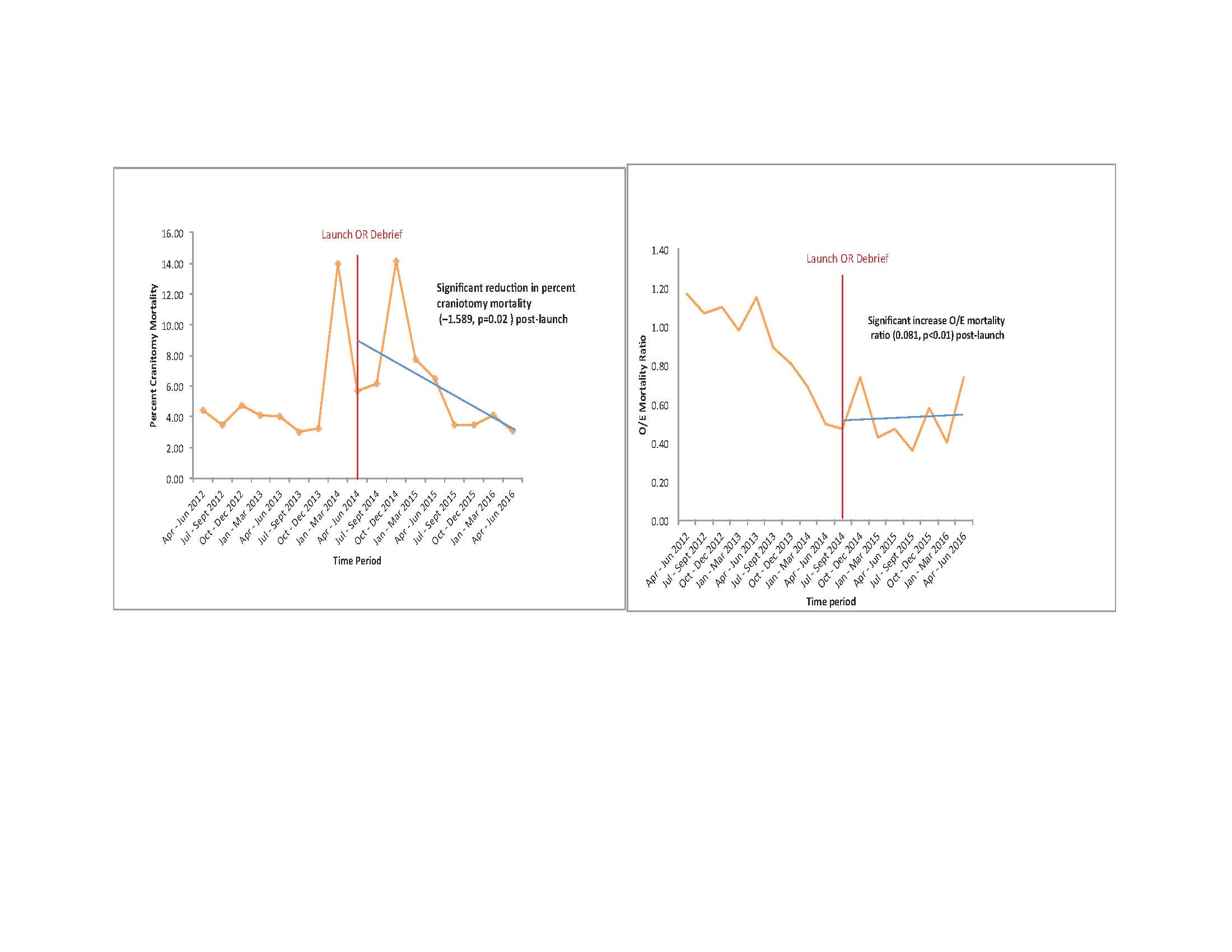
There were no clear trends in patient satisfaction scores as a result of education module prescription. We found divergent results following launch of the OR debrief related to mortality. We noted a significant reduction in the percent craniotomy mortality following launch of the OR debrief (p=0.02) and significant increase in overall mortality observed-to-expected (O/E) ratio (p<0.01) during the same time period (Figure 1); however, overall mortality O/E remained less than 1. There were no significant changes in 30-day readmission rate, length of stay index, direct cost index, and perioperative VTE and hematoma rates due to the OR debrief. We also found no clear trends between completion of individual elements of the ABC checklist and patients’ clinical outcomes.
Conclusions: A hospitalist-led neurosurgery quality improvement collaborative was successful at launching three evidence-based interventions across five medical centers to standardize care. Overall, these interventions did not significantly impact patient clinical and satisfaction outcomes.