Background: Testing of ascitic fluid is recommended in all patients admitted to the hospital and delay in paracentesis has been shown to increase in-hospital mortality. Academic hospitalists in collaboration with internal medicine residency programs are establishing medicine procedure services to address concerns about resident training in procedures and patient safety. Our aim in this study was to examine if the institution of medicine procedure service had any effect on the time between a patient’s hospital admission to paracentesis and a patient’s length of stay in hospital.
Methods: At an 865-bed tertiary care teaching hospital, an inpatient medicine procedure service was introduced on July 1, 2016. This procedure service was staffed by a hospitalist and 1-2 second-year internal medicine residents from 7:00 to 17:00, 7-days a week. To identify patients who had paracentesis performed, we queried our electronic medical records for all fluid samples labeled peritoneal fluid from July 1, 2016 to April 30, 2019 and excluded outpatient paracentesis. Data on age, gender, race, ethnicity, date and time of hospital admission, admitting medical service, presence of spontaneous bacterial peritonitis (SBP), and discharge date and time were retrieved. Patients who had paracentesis performed by a service other than the procedure service during the study period were used as concurrent controls to address secular time trends in outcome measures. We examined two outcome variables: 1) length of stay and 2) time from admission to the procedure. Because both outcome variables were right-skewed, we used generalized linear models with gamma distribution and log-link. To take into account the time trends, we included time in months in the model. Models were adjusted for age, gender, race, whether the admission was during day or night, and the presence or absence of SBP.
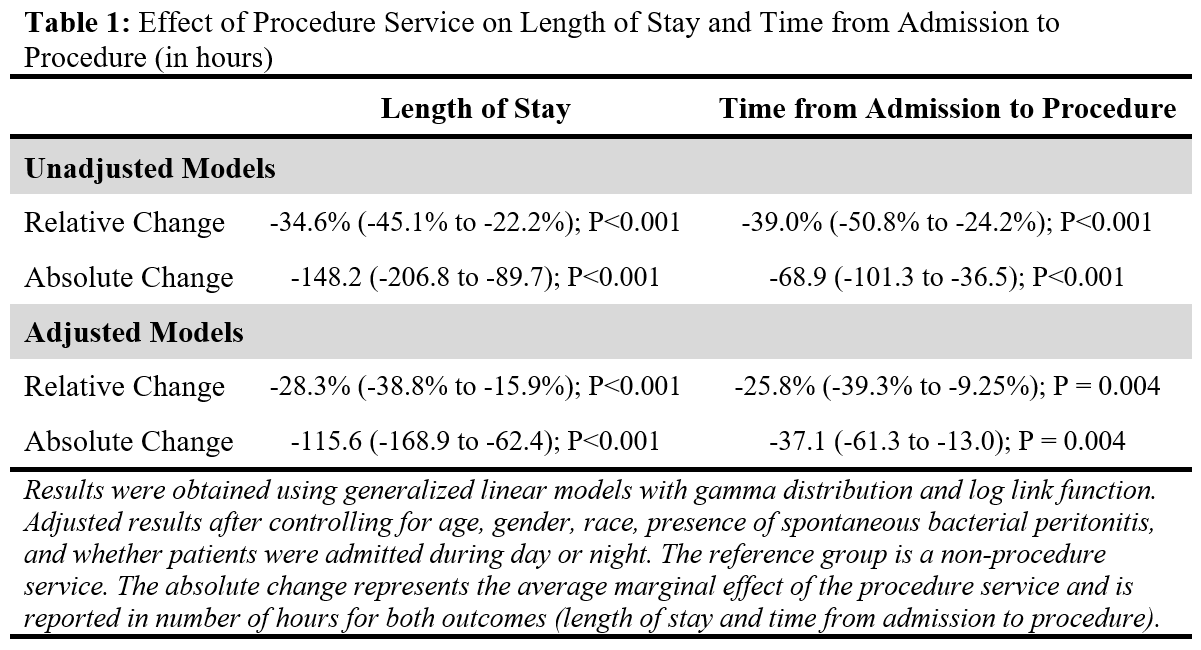
Results: Of the 1694 procedures, 561 (33%) were performed by the procedure service. The mean age of the participants was 54.5 (13.8) years, 925 (54.6%) were Caucasians, 632 (37.3%) were females, and SBP was present in 70 (4.1%) patients. There was no difference by age, gender, time of admission, or the presence of SBP in peritoneal fluids in patients who underwent paracentesis by procedure service versus controls. More Caucasians underwent paracentesis by the procedure service than by non-procedure service (59% vs. 52%, P=0.01). The length of stay and time from admission to the procedure were significantly lower for patients who underwent paracentesis by the procedure service than controls. In adjusted analyses, procedure service resulted in a 28.3% (95%CI= -38.8 to -15.9; P<0.0001) decrease in length of stay and 25.8% (95%CI=-39.3% to -9.5%; P<0.004) decrease in time from admission to paracentesis (Table 1). This relative decrease translates into -115.6 (-168.9 to -62.4) fewer hours in length of stay and -37.1 (-61.3 to -13.0) fewer hours between admission to the paracentesis.
Conclusions: Hospitalist-run teaching procedure service results in a decrease in length of stay and time from admission to paracentesis despite being available only during the day. The decrease in both outcomes was independent of potential confounders and secular time-trends. To our knowledge, this is the first study that demonstrates the benefit of hospitalist-run procedure service in decreasing the length of hospitalization and in shortening the time from admission to the procedure.