Background: In Japan, a “super-aged” society, the rate of end-stage dysphagia in the elderly is increasing. Artificial hydration and nutrition (AHN) can be used for such patients, although it may not improve mortality or quality of life. The many downsides of AHN are not always well explained to patients and their families, resulting in routine initiation of AHN without necessarily reflecting what the patient or their family would want. We evaluate the impact of detailed and precise counseling on the decision towards AHN.
Methods: We enrolled patients ≥ 65 years old with principal diagnosis of aspiration pneumonia, hospitalized during a six-month period. Within this population, those whose dysphagia was too severe to get enough oral intake according to speech therapist’s evaluation were registered as intervention group. A similar population from the previous year were included as a control group. The intervention group received detailed and precise counseling on AHN; the control group were treated conventionally. The rate of aggressive AHN (including enteral nutrition and total parenteral nutrition) was compared between groups. Post-counseling questionnaires were also obtained.
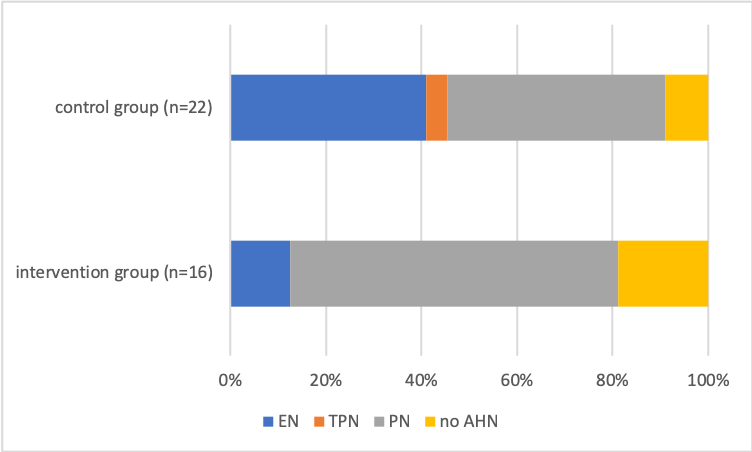
Results: Questionnaires revealed the counseling was considered worthwhile. Aggressive AHN was started by ten out of 22 patients in control group, and two out of 16 patients in intervention group. There was a tendency of less aggressive AHN initiation in intervention group (odds ratio, 5.57).
Conclusions: Counseling on AHN may have a positive impact on reduction of futile AHN care for super-aged patients and outcomes may better reflect their or their family’s true desires.