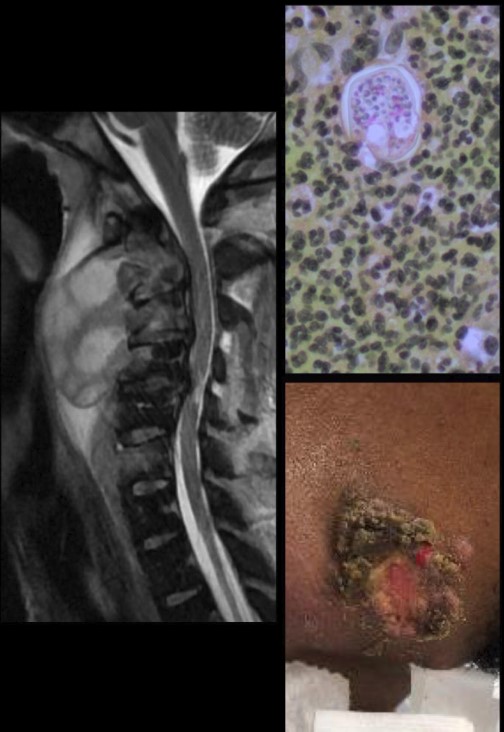
Case Presentation: Coccidioidomycosis is a highly variable disease endemic to the southwest with 60% of infected individuals remaining asymptomatic or suffering mild respiratory illness. Less than 1% of cases result in life-threatening dissemination with immunocompromised hosts being most at risk. We present a rare case of multifocal disseminated coccidioidomycosis (DC) in an immunocompetent young male from a non-endemic region.A 35 year old previously healthy African American male from Virginia presented with persistent multiple skin abscesses on his face and neck with purulent drainage, neck pain and right foot pain for 2 months accompanied by a 20 lb weight loss. He was febrile with a temperature of 102.8F and tachycardic. There was localized crusting and purulent drainage at the right mandibular body and anterior neck. Large, tender fluctuant masses were noted throughout the anterior neck coupled with cervical lymphadenopathy. A neck Computed Tomography (CT) scan revealed a large retropharyngeal abscess extending from C2 to the T1 vertebrae, osseous erosion into cervical spine at C2 through C6 with anterior cervical and ventral epidural abscesses, and multiple bilateral neck abscesses. The patient underwent a C3-C6 decompressive laminectomy and bilateral neck exploration with washout of abscesses. Subsequent imaging identified bony destruction of several ribs and abscessed tenosynovitis of the right ankle. Fungal culture from neck and ankle abscesses grew Coccidioides immitis. An acquired immunodeficiency syndrome and immunoglobulin workup was negative. A genetic testing panel for mutations in the gene encoding signal transducer and activator of transcription 3 (STAT3) was negative. Liposomal amphotericin B (AmB), itraconazole, and interferon gamma 1b (INF-y) were used as treatment for multifocal DC. A 7 week hospital course was complicated by recurrent and metastatic C. immitis infections involving widespread multifocal areas of bony destruction and isolated cutaneous lesions. Despite aggressive treatment our patient passed from overwhelming infection.
Discussion: Our case illustrates an unexpected presentation of DC – an immunocompetent patient from a non-endemic region. Male gender, African American or Filipino race, and those living in endemic areas have a much higher incidence of dissemination. The skin is the most common extrapulmonary site of endemic mycosis with systemic symptoms being largely absent. Rare genetic defects in the STAT3 family of proteins coding for INF-y have been implicated in this process. Mutations in STAT3 coding for INF-y are postulated to cause infectious, dermatologic, skeletal and immunologic features of this disease. Diagnosis of DC usually relies upon serologic testing. However, in patients with early disease- especially those with severe infection-isolation of Coccidioides in culture may be needed to establish the diagnosis because serologic tests for DC become positive at variable periods after onset of illness. Treatment depends on severity of infection. In severe invasive osseous disease, AmB is the main antifungal used and can be combined with fluconazole or itraconazole. Combination therapy with antifungals and IFN-y, as attempted in our patient, have been reported with success in a small case series.
Conclusions: Our case represents an exceedingly rare presentation of an uncommon illness in an unlikely clinical setting – and stresses the importance of culture to make a swift diagnosis and start treatment rather than relying on serologies.