Background: In the United States, vulnerable communities experience significant health disparities, which are largely driven by various social, economic, and environmental factors. Addressing these disparities requires a multifaceted approach and reinforces the need to equip healthcare providers with the needed awareness, competence, and expertise. Given that resident physicians represent a significant proportion of frontline healthcare providers and the future healthcare workforce, enhancing their perspectives and understanding of such disparities can be pivotal in fostering equitable healthcare.
Purpose: The “Equity in Healthcare” course is designed with a clear agenda of empowering resident physicians with the knowledge and skills necessary to comprehend and effectively address health disparities prevalent among underserved populations. The curriculum is devised to bolster their confidence and capability in handling diverse health scenarios pertinent to various underserved groups. Further, it aims to impart lessons in value-based healthcare delivery, fostering an environment of equality and justice in health practices.
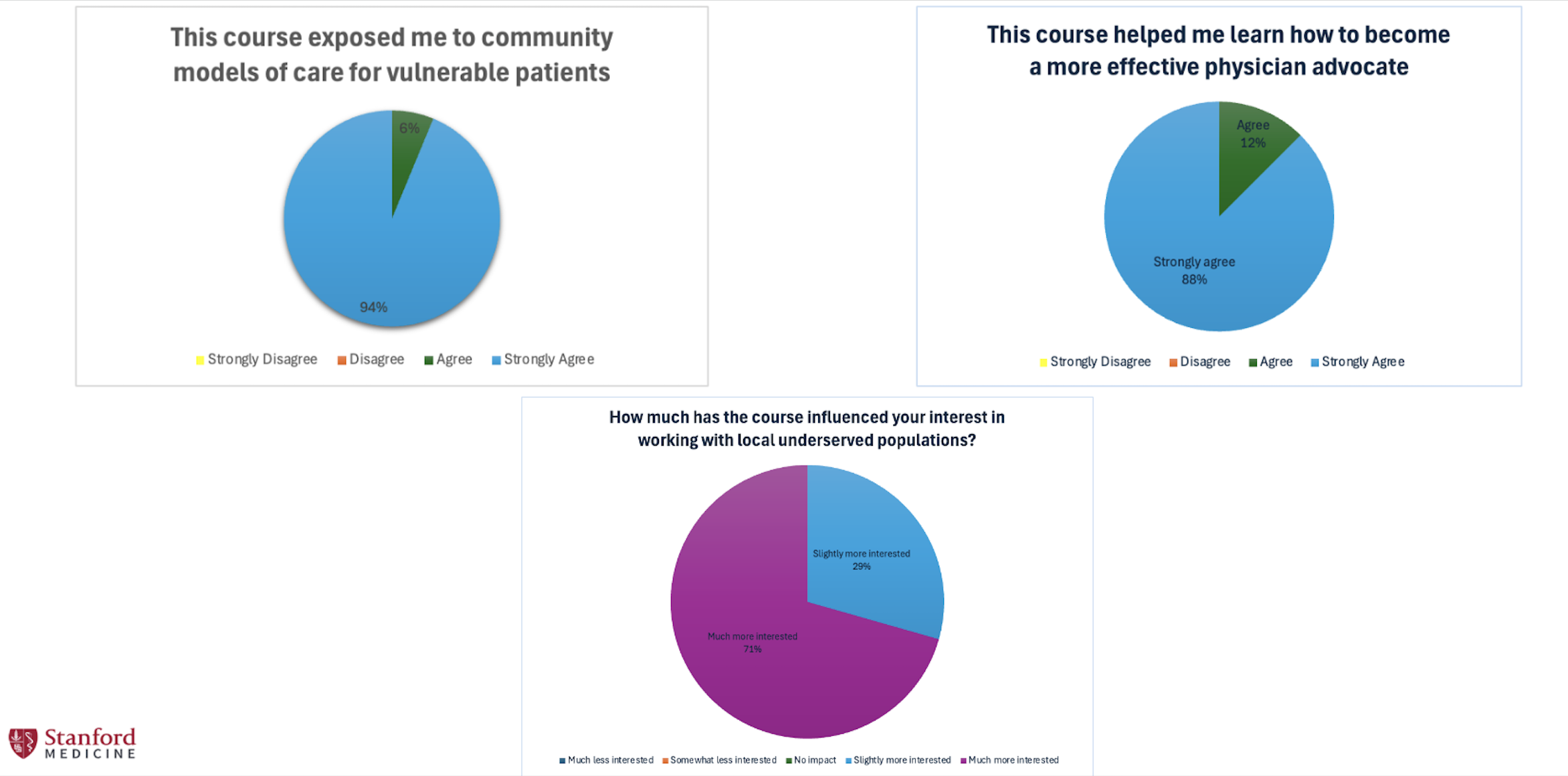
Description: Description: Based on Kern’s 6-step model – a well-recognized model for curriculum development – the “Equity in Healthcare” program entails a comprehensive two-week rotation involving lectures, workshops, and site visits. The course structure strives to enhance understanding of health challenges faced by underserved populations and foster patient-centered advocacy skills. As a part of the rotation, residents are exposed to the unique health needs of subgroups like the incarcerated, LGBTQ+, and those with limited English proficiency. Progress and effectiveness are measured using a combination of formative and summative assessments including Likert scales, open-ended free texts, and pre- and post-rotation assessments.Results: Based on pre- and post-rotation assessments, residents reported significantly improved ability to describe how social determinants of health affect quality of care (P = 0.0005), to identify resources to assist patients experiencing housing instability (P = 0.0001), to incorporate a patient’s social risk into the medical plan during hospitalization (P = 0.0039), and to identify health challenges faced by incarcerated patients (P = 0.0001). Residents also noted a significant improvement in their interest to work with local underserved populations following the rotation (P = 0.0049).
Conclusions: Conclusion: Initial implementation and feedback from this course have been encouraging, with residents reporting significantly improved understanding, confidence, and interest in treating underserved populations. This program has not only succeeded in enhancing resident physicians’ capacity to understand and advocate for multi-faceted health challenges but also bridging the gap between their clinical experiences and the complexities of healthcare disparities. This tested and validated approach serves as a scalable model for educating future clinicians, underscoring its potential to apply to larger student cohorts and amplify its impact on healthcare delivery systems.