Background: Diagnostic errors have been cited as a potential contributor to hospital readmissions, particularly early readmissions (e.g. within 7 days), but little is known about their frequency and characteristics. We performed structured chart review of all medical patients readmitted within 7 days of discharge from a single academic medical center to describe the prevalence of diagnostic error and characterize contributing factors.
Methods: Our study included all patients discharged from the inpatient medical service and re-admitted to our urban academic medical center within 7 days to any service from 1/1/18-9/30/18. A structured review of the electronic medical record was completed independently by two trained board-certified internists, supported by consensus review in discrepant cases. Diagnostic errors were identified using the “Safer Dx Instrument,” a validated tool to identify diagnostic error in primary care visits. When identified, errors were then characterized using the Diagnostic Error Evaluation and Research (DEER) taxonomy tool, an error classification system. Multiple contributing factors could be identified in the same admission. For all identified diagnostic errors, the discharging physician(s) from the index admission were contacted to provide further details of the clinical decision-making and circumstances that may have contributed to the error, which was then used to refine diagnostic error characterization.
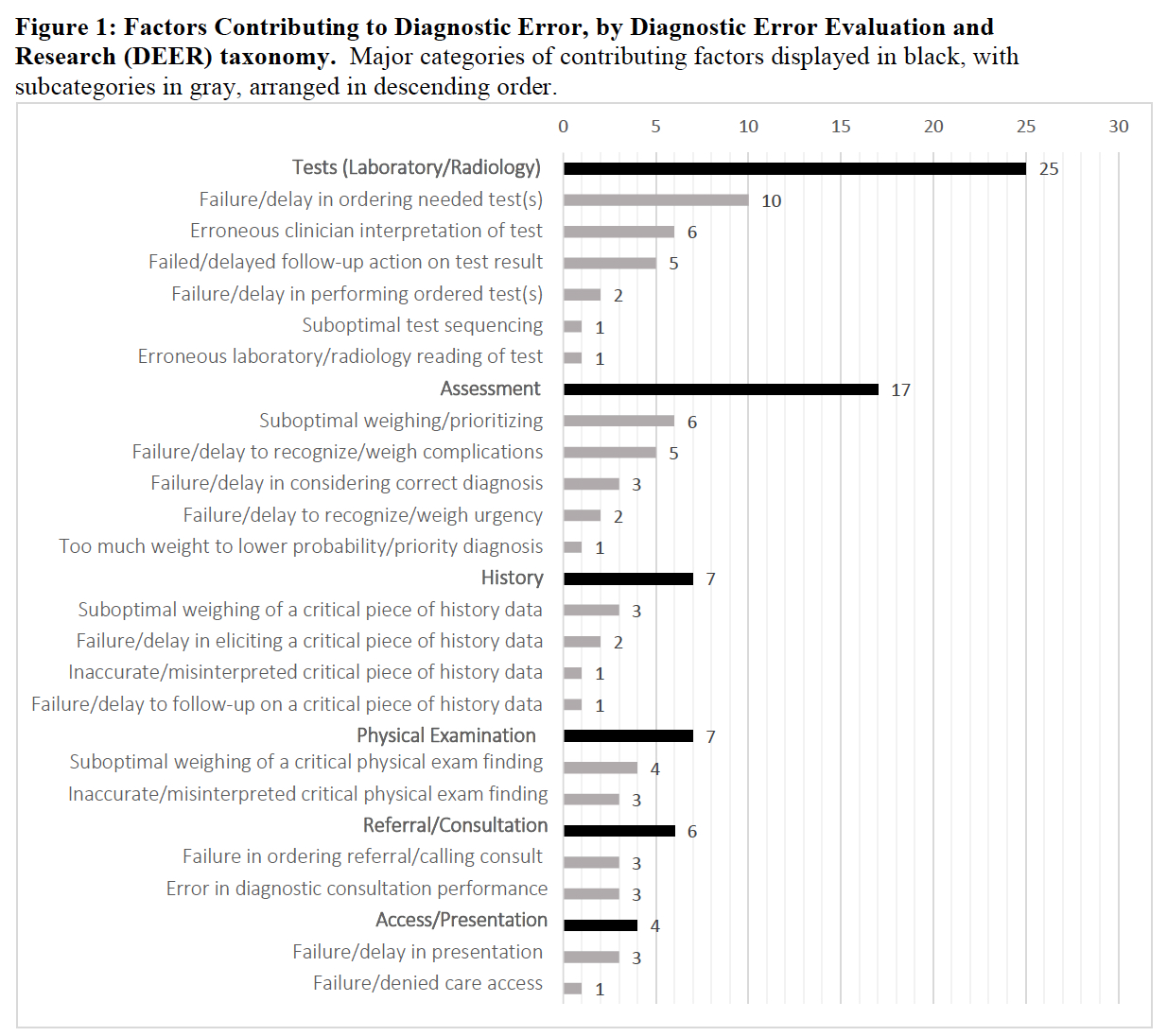
Results: During the study period, of 5663 admissions to the medical service, we identified 261 cases of 7-day readmission (4.6%), of which 258 (98.9%) were reviewed. A total of 18 (7.0%) admissions contained diagnostic error. In 17 of the 18 cases (94.4%), the error was judged as having “moderate” impact, such as short-term morbidity, increased length of stay, or invasive procedure, and 1 had no impact. In the DEER taxonomy, the most common culprit areas within the diagnostic process contributing to error were in Laboratory/Radiology Tests (25) and Assessment (17) (Figure 1). The most common subcategories contributing to error were failure/delay in ordering needed test(s) [10, 56%], erroneous clinician interpretation of test(s) [6, 33%], and suboptimal weighing/prioritizing [6, 33%] (Figure 1). Diagnostic errors represented a breadth of diagnoses; no single diagnosis was repeated among the 18 identified errors.
Conclusions: The prevalence of diagnostic error among 7-day medical readmissions was 7%, similar to prior estimates. Nearly all diagnostic errors had moderate clinical impact. Identified diagnostic errors represented a breadth of diagnoses; thus, disease-specific diagnostic improvement efforts may be of limited utility. The most common underlying drivers of diagnostic error were related to clinician diagnostic reasoning, highlighting the importance of efforts to improve diagnostic reasoning.