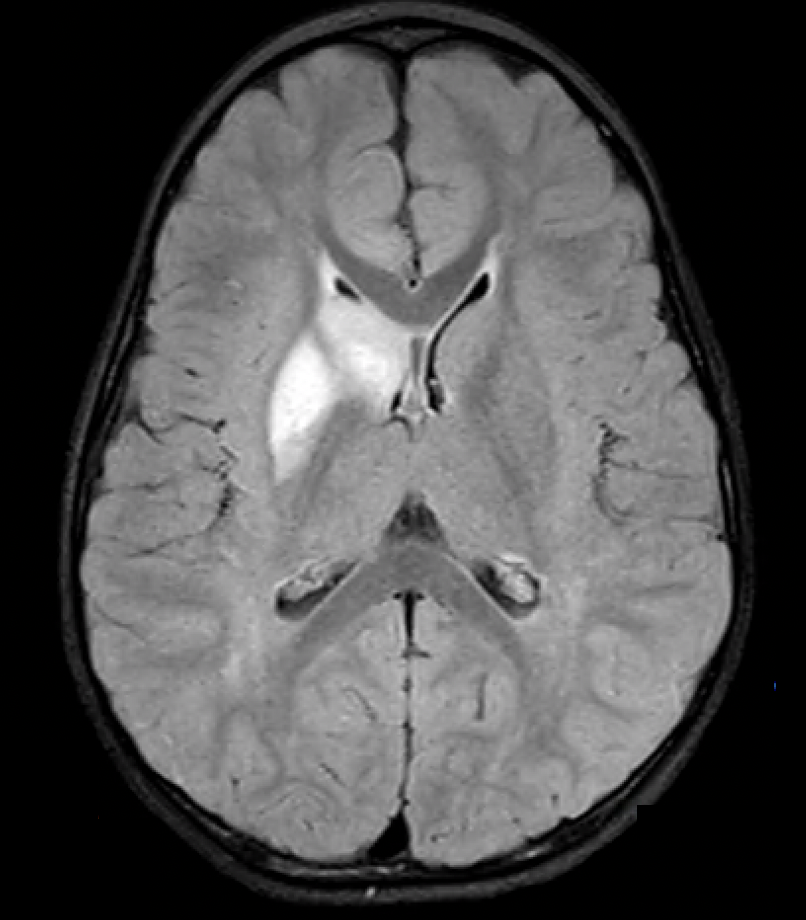
Case Presentation: A two–year-old previously healthy boy presented with the chief complaint of acute onset left-sided weakness in the setting of recent fever and upper respiratory symptoms. Admission exam was notable for left-sided facial droop, weakness of upper and lower extremities, and inability to walk. Initial CT head was notable for a right basal ganglia hypodensity. Subsequent CTA and MRI of the head suggest focal cerebral arteriopathy (FCA) leading to infarct in the right anterior cerebral artery (ACA) and middle cerebral artery (MCA) without signs of moyamoya disease. Infectious workup revealed presence of parainfluenza and rhinovirus/enterovirus by PCR and reassuring CSF studies. Neurosurgery determined surgical intervention was not indicated, and the patient was initiated on aspirin therapy. Three weeks later, he was readmitted with new right-sided deficits, focal seizures, and new collaterals on imaging consistent with interval development of moyamoya disease leading to initiation of pulse-dose steroids. Repeat infectious and viral PCR testing identified acute influenza without signs of herpes or varicella infection. Echocardiogram, hypercoagulability workup, and moyamoya genetic panel were normal. Throughout both admissions, he was managed by the hospital medicine service after initial stabilization by the ICU. Recovery period was complicated by hypertension, dysphagia, emotional lability, and persistent residual weakness of upper and lower extremities requiring inpatient rehab.
Discussion: Pediatric arterial ischemic stroke (AIS) is rare. Despite young age, children suffer significant mortality and morbidity, with more than half of survivors suffering ongoing neurologic deficits with arteriopathies such as moyamoya disease and FCA representing up to an estimated 50% of those cases. Studies have also indicated a significant risk of recurrence in arteriopathies compared to other types of AIS. Moyamoya disease, the idiopathic variant, is characterized by narrowing and occlusion of the internal carotid artery (ICA), MCA, and ACA that is historically described as “puff of smoke” on imaging and leads to focal deficits. Seizures, as seen in our case, are common and can be the initial presenting symptom. Pathophysiology of moyamoya disease is still poorly understood with current hypotheses suggesting possible infection, immune, environmental, and inherited factors. Moyamoya disease has also been reported to present with initial unilateral focal cerebral arteriopathy that then progresses, further complicating diagnosis.
Conclusions: We present an unusual case of pediatric stroke. Initially presumed to represent a focal cerebral arteriopathy triggered by viral infection, subsequently our patient suffered a recurrence leading to a diagnosis of moyamoya disease. This case is unusual not only in its progression on imaging but its association with viral disease. Given the otherwise unremarkable workup, we hypothesize repeat upper respiratory infections (URI) may have been the trigger. Previous studies have identified an increased risk with recent URI in cases of FCA. Enterovirus infection leading to FCA has been reported, but we were unable to identify any cases in the literature noting parainfluenza or influenza leading to either FCA or moyamoya disease, suggesting these may be newly discovered risk factors. This case emphasizes the heightened awareness needed for this rare disorder and need for future study on association between viral infections and cerebral arteriopathies.