Background: Each year, over 5 million hospital-to-skilled nursing facility (SNF) transitions occur; of these patients, 20% are readmitted within 30 days. SNF transitions can be complex and error-prone, with hospital medicine teams noting unfamiliarity with key handoff information and SNF providers reporting incomplete or inconsistent discharge information. While effective communication between hospital and SNF providers can reduce readmission rates, there is currently is no standardized handoff approach.
Purpose: To develop a standardized method of discharge communication between resident hospital medicine teams and SNF providers.
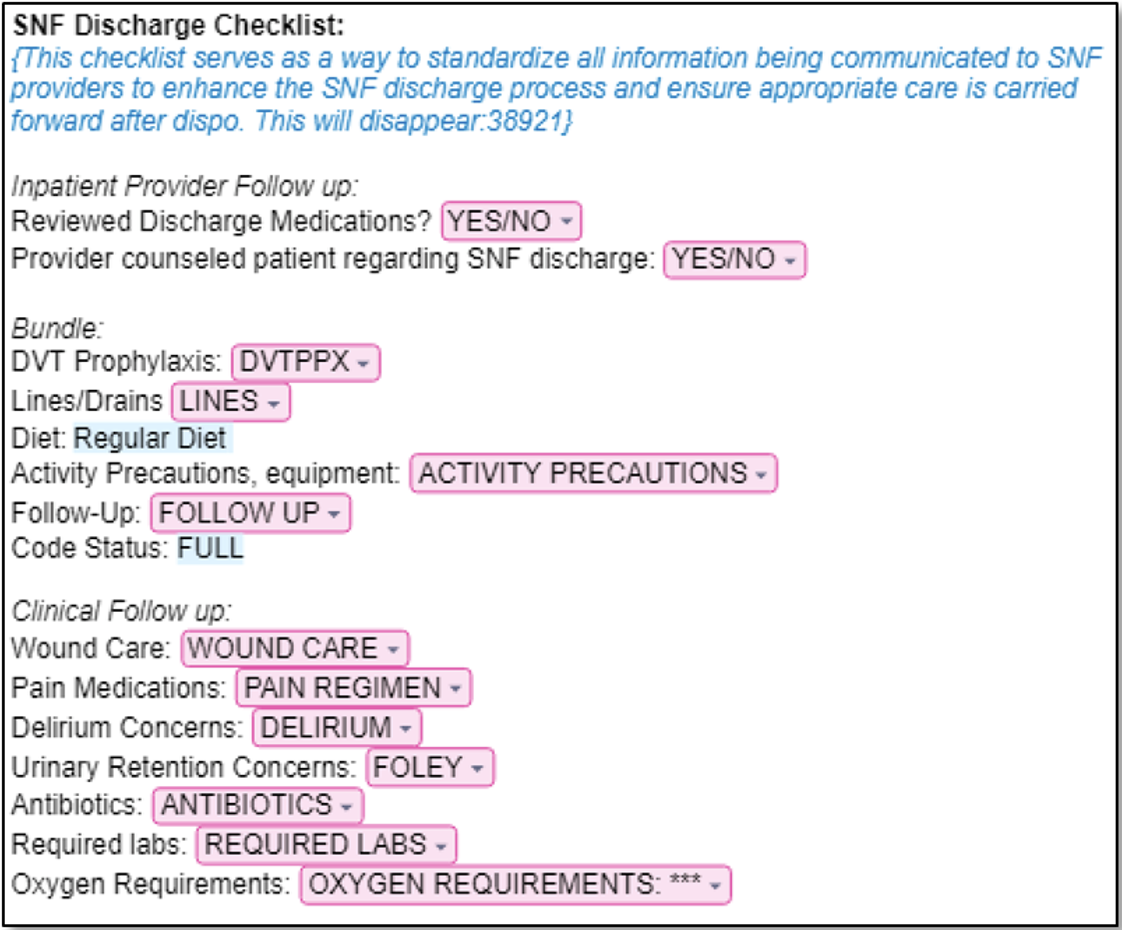
Description: PHASE 1: NEEDS ASSESSMENT In September 2023, our resident-led quality improvement team surveyed internal medicine residents on the medicine teaching service (n=53) and providers at two local SNFs (n=11) to better understand the gaps in SNF discharge communication. 40% of residents did not feel confident in knowing what to include in their documentation to SNF providers and only 31% of residents were comfortable counseling patients about what to expect at a SNF. 75% of SNF providers were confident that the discharge summary would contain a clear hospitalization summary but less confident about it including an adequate pain regimen (60%), follow-up referrals (58%), and wound care recommendations (54%) (Figure 2). PHASE 2: DEVELOPMENT OF SNF DISCHARGE CHECKLIST Through survey results and collaboration with SNF clinicians and hospital-based case managers, nurses, and clinicians, we designed a standardized SNF discharge checklist for resident teams in the form of an electronic health record (EHR)-based dotphrase. The dotphrase prompted residents to insert key information, such as wound care recommendations (Figure 1). Residents were initially asked to manually include this dotphrase (.SNFDischargeChecklist) at the top of discharge summaries for patients discharging to SNF and review it during verbal handoffs to SNF providers. PHASE 3: TACTICS TO INCREASE UTILIZATION Following the dotphrase launch, our team utilized awareness campaigns, monthly emails, reminder pages, and gamification to encourage dophrase uptake across resident teams. By March 2024, the dotphrase was updated to now auto-populate into all discharge summaries whenever SNF was selected as the discharge location, eliminating the need to manually insert the dotphrase to get the checklist to appear. From October 2023 to May 2024, monthly utilization of the dotphrase increased from 41% to 88%, with a total cumulative utilization rate of 57%. PHASE 4: EVALUATION Residents and SNF providers were re-surveyed 8 months after the dotphrase launch. Compared to the pre-intervention period, significantly more residents reported including key information in the discharge summary. Interpretation of SNF provider surveys was limited by a small sample size. Some SNF providers endorsed smoother hand-offs, but there was room for improvement in counseling patients on realistic expectations around SNF-level care (Figure 2).
Conclusions: Through multidisciplinary collaboration, we created and implemented an EHR-based checklist to address communication gaps in SNF discharge handoffs. This resulted in improving resident knowledge and self-efficacy. Future research could study whether standardized SNF handoff communication decreases medical errors, improves patient safety, and reduces readmission rates.