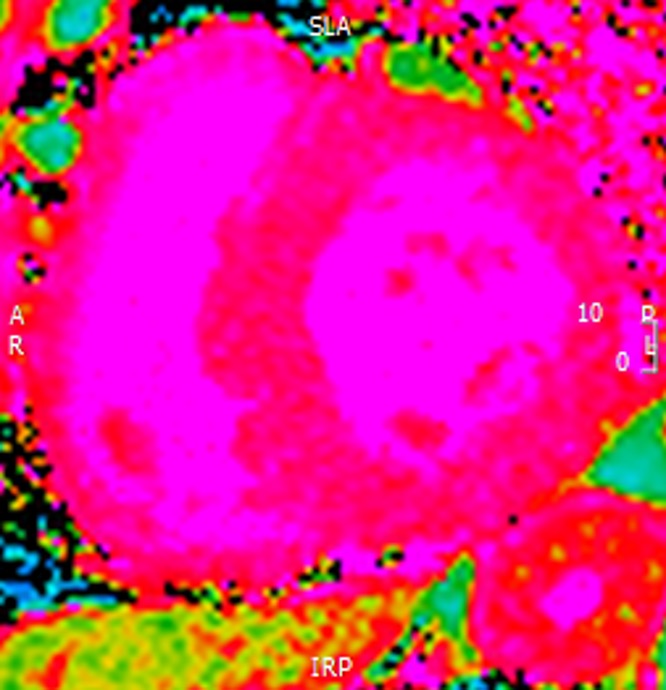
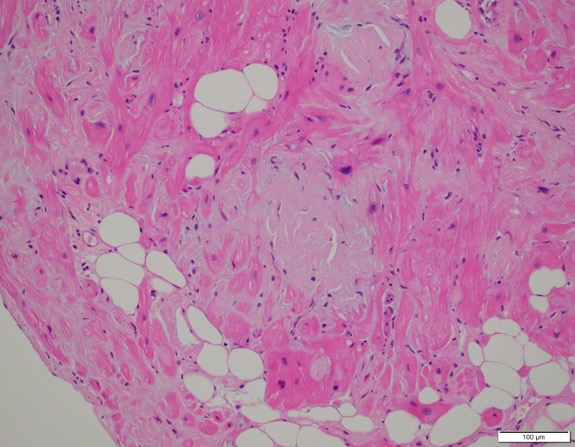
Case Presentation: 66-year-old man with recent diagnosis of heart failure with preserved ejection fraction, atrial fibrillation, and chronic kidney disease presented with worsening shortness of breath. On presentation, he had crackles in the left lower lobe, 1+ pitting edema, and macroglossia. BNP 17,371and creatinine 2.88 (baseline of 2.4). Chest x-ray: mild pulmonary vascular congestion, trace bilateral pleural effusions. Echo showed severe concentric left ventricular hypertrophy with restrictive filling pattern and moderate right ventricular hypertrophy. ECG showed low voltage QRS. These findings are consistent with cardiac amyloidosis. SPECT concerning for infiltrative disease. CMR showed markedly elevated native T1 in the setting of LVH and mildly reduced LV systolic function. Serum protein electrophoresis showed no monoclonal gammopathy. Serum free light chains showed elevated lambda at 722 with kappa of 45 and K/L ratio of 0.06. Bone marrow biopsy: 12% aberrant plasma cells with associated “amorphous eosinophilic material noted predominantly in association with the vessels that is congophilic with apple green birefringence on Congo red stain typical of amyloid.” Fat pad biopsy was attempted but he had a PEA arrest with ROSC obtained. Endomyocardial biopsy showed extensive congophilic interstitial, microvascular myocardial and endocardial deposition. Congo red stain was strong positive with green birefringence on polarization microscopy.
Discussion: Cardiac Amyloidosis (CA) is underdiagnosed yet an important cause of heart failure all clinicians should remember. Amyloidosis is a family of protein-misfolding diseases. In CA, these misfolded proteins fill the extracellular space of the heart leading to a thick, rigid myocardium with restrictive pathophysiology of both ventricles. CA is not an isolated disease, but part of a systemic disease. In particular, AL Amyloidosis infiltrates the kidneys, nervous system, skin, vasculature, and occasionally liver and gastrointestinal system3.Patients present with typical decompensated heart failure symptoms, but peripheral edema is not due to heart failure, rather hypoalbuminemia from nephrotic range proteinuria. Other symptoms of AL amyloidosis include periorbital purpura and macroglossia (seen in about 10%). When diagnosing CA, the gold standard is a tissue biopsy. An endomyocardial biopsy is more sensitive and is preferred over a fat pad biopsy. Congo red stain of the biopsy will stain pink and show apple-green birefringement under polarized microscope with amyloid is present. ECG typically shows a low voltage QRS complex with an unusual axis as an extreme right axis. Echocardiograms show concentric left ventricle thickening. LV wall thickness is typically 15mm or greater. Cardiac MRI with late gadolinium enhancement is the best imaging modality because it shows a typical pattern, but many patients with amyloid, due to decreased GFR, cannot receive gadolinium. Native myocardial T1 CMR can be used to make the diagnosis of amyloid. Greater than 90% of patients having abnormal light chain kappa/lambda ratio but with normal SPEP and UPEP. Immunofixation is more sensitive and shows a monoclonal band.
Conclusions: While not a common etiology of heart failure, in the correct patient with the above constellation of findings, cardiac amyloid should be considered in the differential.