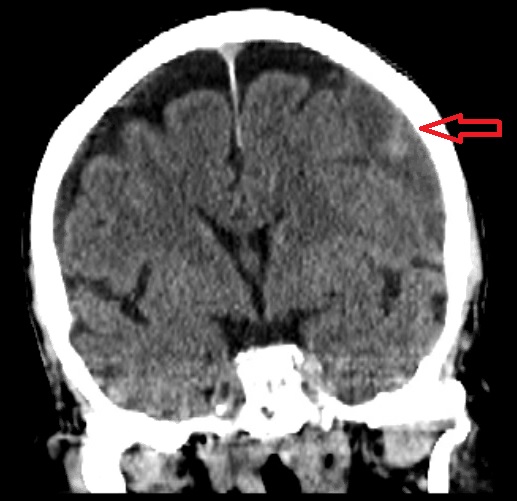
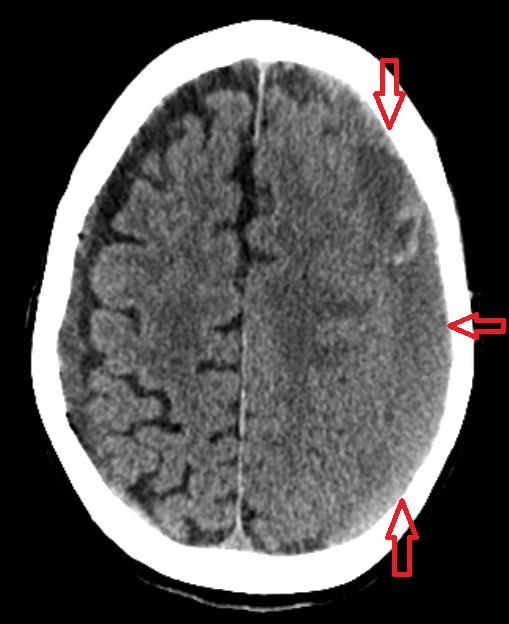
Case Presentation: An 83 year-old female with history of hypertension presented to the emergency department with altered mental status for the past 2 days. Family reported patient to have a low impact fall, 2 weeks prior. In route, patient was noted to be febrile at 101.7˚F. Upon arrival, vitals were stable. Patient was found to have impaired mobility and aphasia. Per family, patient was at her normal baseline health prior. Bloodwork was significant for hyponatremia and electrolyte disturbances. CT head showed acute and subacute and acute on chronic subdural hematomas overlying the left and right cerebral convexities measuring up to 2 cm and 0.8 cm in thickness respectively. Associated mass effect on the left cerebral hemisphere with extensive sulcul effacement and mild 4 mm left-to-right midline shift. Neurosurgical recommendations for burr hole evacuation of subdural hematoma and insertion of drain. During procedure, purulent malodorous bloody was drained and cultures obtained. Meanwhile, blood cultures returned positive for pan-susceptible Salmonella Dublin. Subsequent hematoma cultures were positive for Salmonella, making the post-operative diagnosis subdural hematoma and empyema. Antibiotics were initiated with plan to treat for 8 weeks.
Discussion: We describe an interesting case of salmonella bacteremia complicated by subdural salmonella empyema. Salmonella is a facultative intracellular bacterium that can colonize humans through fecal-oral route transmission. Salmonella Dublin is known to be prevalent on dairy farms in the United States. Pathogenic potential and disease outcomes differ substantially by serotype. Invasive nontyphoidal Salmonella isolated pathogenic serotypes are most commonly Salmonella enteritidis and typhimurium. Salmonella enterica serotype Dublin, is known to have a greater predisposition for causing invasive disease and more likely to cause bacteremia. The clinical presentations can vary between acute and chronic carriers. Symptoms include gastrointestinal manifestations, septicemia or focal infections. Focal intracranial infections are unusual and rare manifestations of salmonellosis. According to literature review, focal infections due to salmonella are very rare and not many cases have been reported in world literature.
Conclusions: We describe a rare case of salmonellosis seeding the brain. Our patient was diagnosed with salmonella bacteremia, resulting in an infected subdural hematoma. Extra-intestinal focal infections are related to host immune deficits and diseased tissue. The mainstay treatment is with antibiotic therapy and surgical debridement, if necessary, to achieve clinical and bacteriologic cure. Invasive non-typhoidal salmonella is an emerging pathogen. The usual suspect is an immunocompromised host. With a better understanding of its ecological and immunological niche and epidemiology, we can create new avenues for public health strategies to prevent infections and minimize transmission. This should also prompt clinicians to have an increased awareness of possible occult immunosuppressive disease in an infected patient with salmonellosis.