Background:
The Veterans Health Administration (VHA) is undergoing a national effort to improve access for its patients so that veterans can get the right care, in the right place, at the right time. National benchmarks suggest a time period of two weeks is adequate for non-acute specialty care follow-up, yet our hospital typically averages third next available appointments more than 20 days from hospital discharge. There are numerous examples in the literature of patient centered medical homes improving patients’ access to medical care, and the VHA is leveraging this model by employing Patient Aligned Care Teams (PACTs). PACT members include family members, caregivers, primary care providers (PCPs), nurse care managers, clinical associates, and administrative clerks.
Purpose:
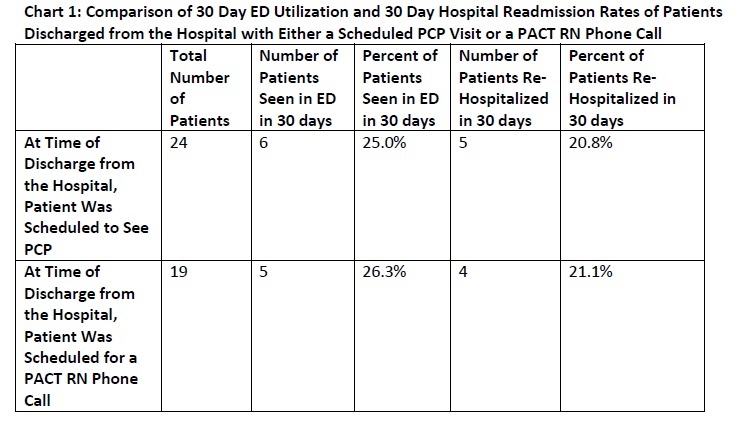
To compare 30 day ED utilization rates and 30 day re-hospitalization rates of patients who were scheduled to receive calls from PACT nurses at the time of discharge versus those provided PCP visit appointments at the time of discharge.
Description:
At our hospital, physicians routinely request PCP follow-up prior to their patients’ hospital discharge, regardless of medical need. We theorized allowing providers to schedule appointments for their patients to receive a “check in” call with a PACT nurse, rather than an in-person PCP visit, would be non-inferior, as measured by 30 day emergency department (ED) utilization rates and 30 day rates of re-hospitalizations. This new approach could increase in person PCP visit availability for patients discharged from the hospital and save other patients the burden of coming to clinic when not medically indicated.
During multidisciplinary discharge planning rounds, inpatient medicine providers were asked if patients of one pilot clinic required an outpatient PCP visit after discharge from the hospital or if a pre-scheduled phone call from a PACT nurse would be appropriate. This phone call triaged patients to in-person visits if medically indicated. We then performed a chart review 30 days after hospital discharge to assess the rates of ED utilization and re-hospitalization. Data collection (Chart 1) is ongoing.
Conclusions:
The PACT model is a promising means to improve veterans’ access to medical care. Preliminary results suggest that the use of the PACT model to have nurses contact patients after discharge from the hospital (rather than the routine use of a post hospital discharge PCP appointment) does not significantly increase the rates of 30 day ED utilization or 30 day hospital readmission. Further study is required to investigate if rates of clinic availability are impacted. We propose further investigation into this model of post hospital discharge follow-up as it may be one means to improve access for veterans.