Background: Discharging patients is a complicated process that requires planning, coordination and communication between multiple care team members. Ideally this process begins at admission and is updated in real time as the patient care plan evolves and discharge needs become known. Discharge plans are often made using some form of static communication, such as in-person multi-disciplinary rounds. These plans become obsolete as care progresses but are not updated until the next multi-disciplinary rounds, a day or more later. Such obsolete discharge plans often create confusion and added work for bedside nurses who need to understand the plan for discharge, and communicate that plan with patients and caregivers. We therefore developed a streamlined communication tool that contains the discharge plan, is updated in real-time, leverages existing clinician workflows, and is readily available from within the electronic medical record (EMR). We hypothesize that such a virtual discharge whiteboard (VDW) will increase nurses’ knowledge of the discharge plan, and allow them to discharge patients as efficiently and safely as possible.
Purpose: To understand the effects of implementing a VDW on nurses’ understanding of, and satisfaction with, the discharge plan.
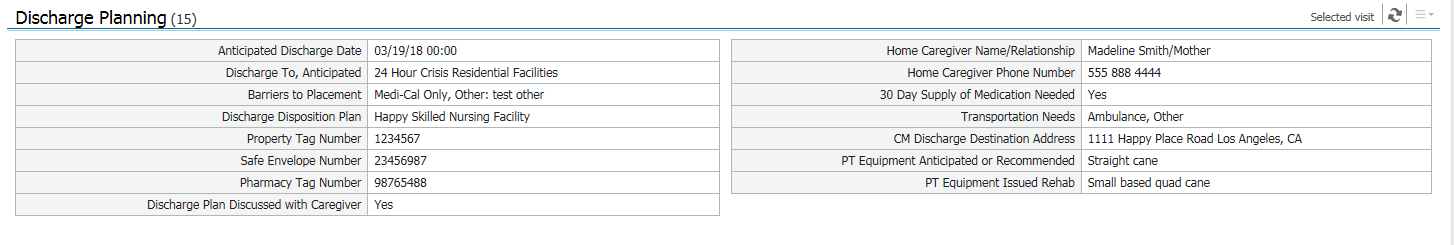
Description: A multidisciplinary team of physicians, nurses, social workers, pharmacists, therapists and IT specialists created the VDW by identifying 15 key pieces of information needed for a comprehensive discharge plan. We also identified who is responsible for providing that information, and how providers could submit that information to the VDW in real time, using existing documentation workflows rather than by creating an additional workflow. We then built the VDW into one easy-to-read page within our EMR (Figure 1). The VDW incorporates input from various members of the care team, including nurses, social workers, therapists, pharmacists and physicians. Additionally, as care plans evolve throughout the course of a hospitalization, and providers update their documentation, the VDW is also updated simultaneously.
A “surprise discharge” – the discharge of a patient for which the bedside nurse had no prior knowledge – is a major nursing dissatisfier and a major cause of inefficient and unsafe discharges. We are studying the impact the VDW has on nurses’ understanding and satisfaction of the discharge process in a quasi-experimental, pre-post study. Baseline data suggest that 73% of surveyed nurses are caught off guard by a discharge at least once per shift and 65% are not confident in their own awareness of their patients’ discharge plans.
Conclusions: A communication tool that gathers the information needed to complete a patient discharge into a streamlined, user-friendly platform within the EMR can improve nurses’ awareness of the discharge plan, and satisfaction with the discharge process.