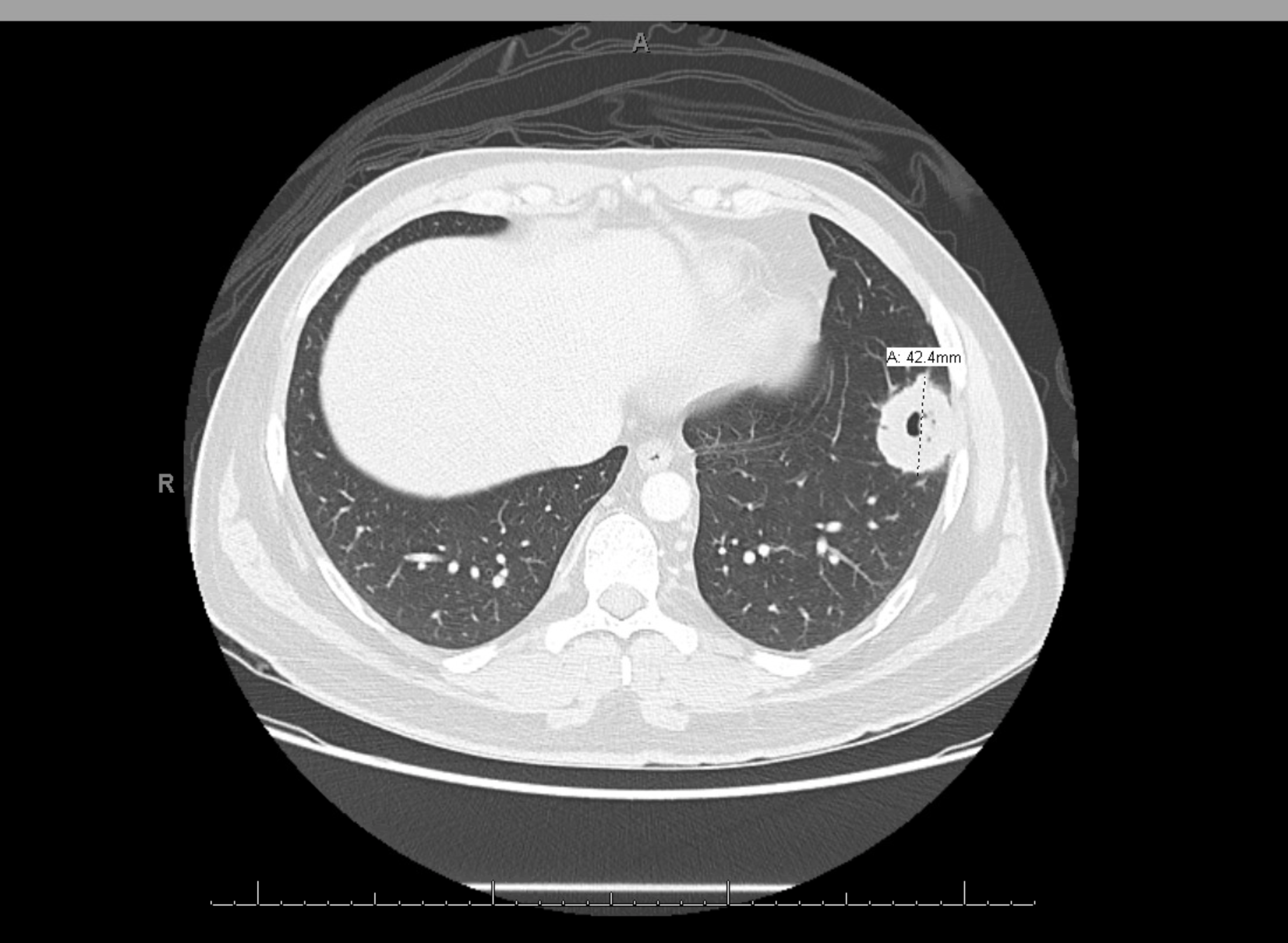
Case Presentation: A 34-year-old male with history of complicated otitis media with bilateral facial palsy presented to the emergency department (ED) with a 1-week history of dry cough, bilateral eye redness and epistaxis. The patient had recurrent episodes of bilateral purulent otitis media over the past 4 months, failing treatment with anti-histamines and antibiotics, and only partially responding to short courses of ster-oids, eventually leading to bilateral facial nerve paralysis. He underwent bilateral tympanostomy and a revision surgery for declining symptoms. No additional work up had previously been done to determine the underlying cause of his recurrent otitis media. In the ED, he denied fever, chills, sinus congestion, sore throat, ear symptoms, hemoptysis, or shortness of breath. Physical examination revealed bilateral chemosis, tympanostomy tubes without drainage and bilateral Bell’s palsy. Coarse rales at the lung bases were auscultated. Laboratory tests were significant for leukocytosis of 12.1 x 109/L, ESR of 49 mm/hr and CRP of 14.28 mg/L. Chest X-ray demonstrated multiple cavitary masses concerning for tuberculous or fungal infection vs autoimmune etiology vs metastases. The findings were confirmed on CT chest. Further work up included negative quantiferon, angiotensin converting enzyme, anti-nuclear antibody, anti-myeloperoxidase antibody, but positive anti-proteinase-3 anti-neutrophil cytoplasmic antibody (21.0 U/mL, reference ≤ 0.9 U/mL), high titers of IgE (347 IU/ml, reference <=164 IU/ml) and active urinary sediments with 68 RBC per high power field. The patient underwent lung biopsy of one of his nodules which showed necrotizing granulomas with multinucleated giant cells consistent with GPA. He was started on prednisone and IV rituximab. His symptoms markedly improved over the next few months with significant decline in his inflammatory markers.
Discussion: GPA is a systemic disorder of small to medium vessel vasculitis causing necrotiz-ing granulomatous inflammation. Patients with GPA commonly have widespread clinical symptoms, including involvement of ear, nose and throat (up to 90% of cases), kidneys (~85%), lungs (~50%), skin (~50%), eyes (~33%), nervous system (~33%) etc. ENT manifestations in GPA represents most frequent symptom at the onset of the disease but isolated otological involvement without any other systemic signs is uncommon which can lead to delay in diagnosis with patients ex-periencing protracted symptoms and complications. We recommend that otitis media/otomastoiditis refractory to standard treatment should warrant further investiga-tion for uncommon causes such as GPA. Timely diagnosis and treatment with immunosuppressants can prevent complications such as permanent hearing loss and facial nervy palsy.
Conclusions: Granulomatosis with polyangitis (GPA) is an uncommon systemic vasculitis typi-cally present in elderly with widespread clinical manifestations involving the ears, nose and throat (ENT), lungs, kidneys, skin, eyes, nervous system although this disease has been reported in all age groups. GPA patients may be younger with isolated otological symptom posing a diagnostic challenge to the clinicians.