Case Presentation: Dissseminated intravascular coagulation (DIC) can present as excessive bleeding or involving thromboembolic event. Here in we report a case of 68 year old woman with leukemia presenting in both spectrum of disease.
A 68 year-old woman presented with weight loss, fever, and rash. Laboratory studies revealed white count 84 k/µL cells, hemoglobin 8.9 mg/dL, and platelets 98 k/µL cells. Bone marrow biopsy revealed immature B-lymphoid and myeloid cells, consistent with acute bi-phenotypic leukemia, with positive Philadelphia chromosome mutation. Treatment was initiated with hydoxyurea, appropriate chemotherapy regimen, empiric intra-thecal methotrexate, and dasatinib. On day four of admission patient was found to have word finding difficulty and CT scan of head revealed left temporal lobe infarct. On day six, she had partial thromboplastin time (PTT) >200 seconds, international normalized ratio (INR) 2.6, prothrombin time (PT) 27 seconds, fibrinogen < 70mg/dL, and platelets 24 k/µL cells concerning for DIC. Treatment with low dose fractionated heparin (UFH) and cryoprecipitate was initiated. Patient exhibited no bleeding complication, and repeat CT head of the brain negative for intracranial bleeding or new stroke.
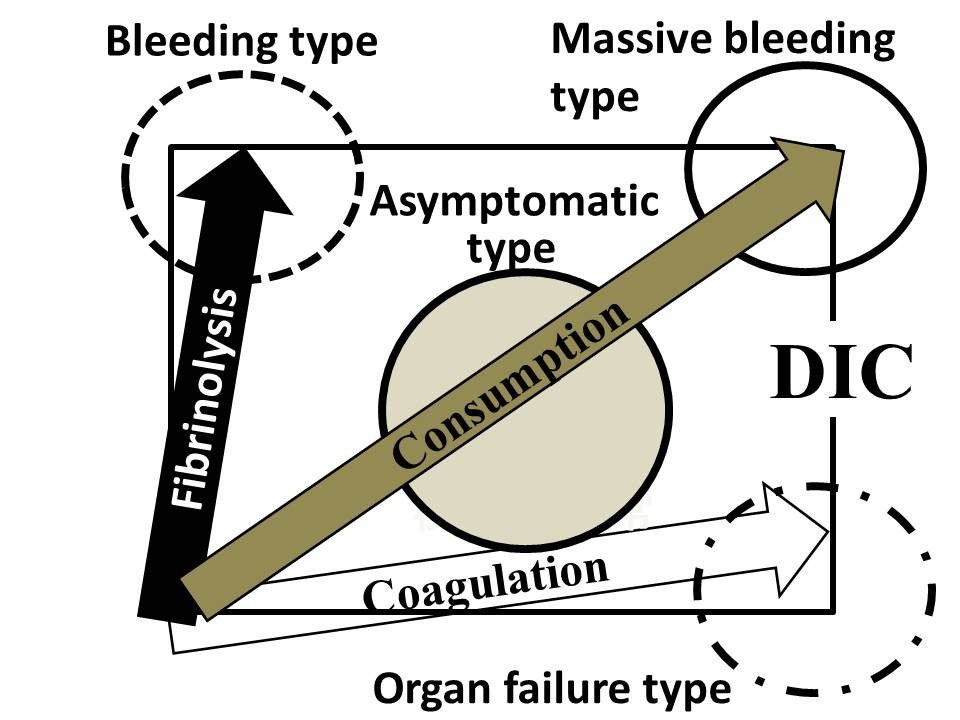
Discussion: DIC is the result of hypercoagulation, hyperfibrinolysis, or both processes simultaneously. The four major types of DIC are characterized by the presence or absence of hypercoagulation and hyperfibrinolysis. In hyperfibrinolysis-dominant DIC, bleeding is the primary symptom; this type is often seen in patients with acute promyelocytic leukemia. In hypercoagulation-dominant DIC, organ failure is the main symptom; this type is often seen in sepsis. When both hypercoagulation and hyperfibrinolysis are present, there is usually massive hemorrhage, often seen after major surgery. When there is weak hypercoagulation and weak hyperfibrinolysis, there are often no clinical symptoms, although abnormalities in clinical laboratory tests are observed; this type of DIC is called the non-symptomatic type of DIC or pre-DIC. Our patient was challenging, as she was at very high risk of thrombosis and bleeding at the same time. Her initial presentation was consistent with thrombosis-predominant organ failure type manifesting as stroke. But later her disease shifted to the pre-DIC type with risk of conversion to bleeding type. There is precedent for low dose heparin to raise fibrinogen to normal range, along with aggressive blood product and platelets replacement. Prior to the development of all trans retinoic acid (ATRA) for DIC management, heparin was used to treat DIC. Currently, UFH (unfractionated heparin) is preferred in treatment of sepsis-associated DIC to manage pro-thrombotic risk.
Conclusions: The management of DIC is difficult. Diagnosis and treatment of DIC is complicated by the fact that the types of DIC may shift or change. The mainstay of DIC treatment is treating the underlying cause, such as leukemia in our patient. Acute management of DIC should be carried out based upon the active DIC type.