Background: Asthma, bronchiolitis, and pneumonia are common pediatric inpatient diagnoses. Viral testing (VT) is not routinely necessary for these diagnoses as it often does not impact management. Our study objectives for each diagnosis are to; 1) describe trends in VT over the last 5 years including seasonal variation (respiratory season- Oct-March versus non-respiratory season- April-Sept), 2) describe the rate of VT associated with individual hospital cohorting practices and 3) describe the rates of VT associated with individual hospitals’ presence of clinical pathways and electronic medical record (EMR) order sets.
Methods: This is a retrospective chart review using Pediatric Health Information System (PHIS) database over the last five years (2014-2018). Patients 0-18 years, admitted to a children’s hospital with the primary or secondary diagnosis of either asthma, bronchiolitis, and/or pneumonia were included. Patients flagged with complex chronic conditions, prolonged hospital stay of >7 days, or pediatric intensive care unit stay were excluded. A hospitalist from each PHIS hospital was surveyed about their institution’s VT practice patterns, specifically the presence of cohorting, and the use of clinical pathways and/or EMR order sets for asthma, bronchiolitis, and pneumonia. The data was summarized using frequency and percent for categorical variables, and mean and standard deviation for quantitative variables. The Chi-squared and Wilcoxon rank-sum tests were used to test for associations.
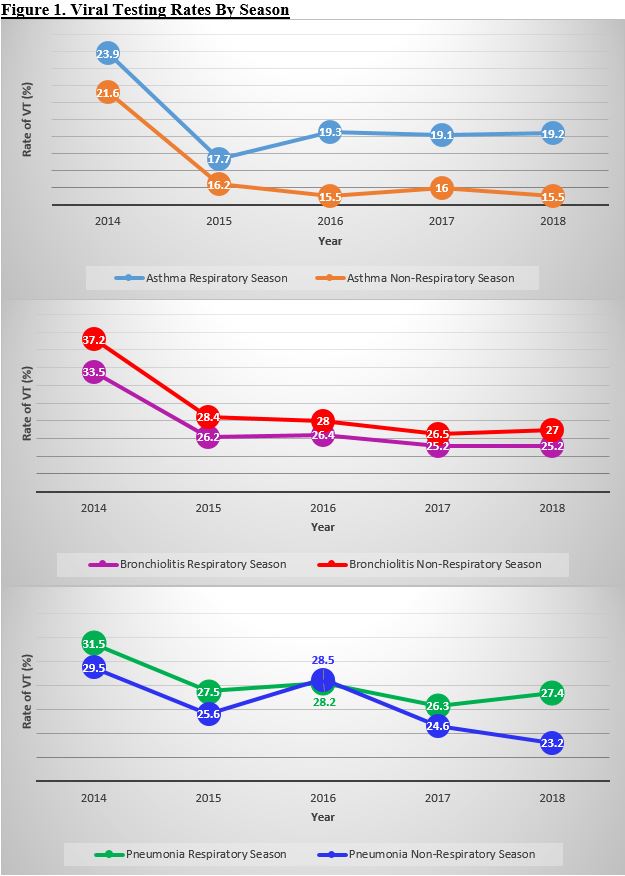
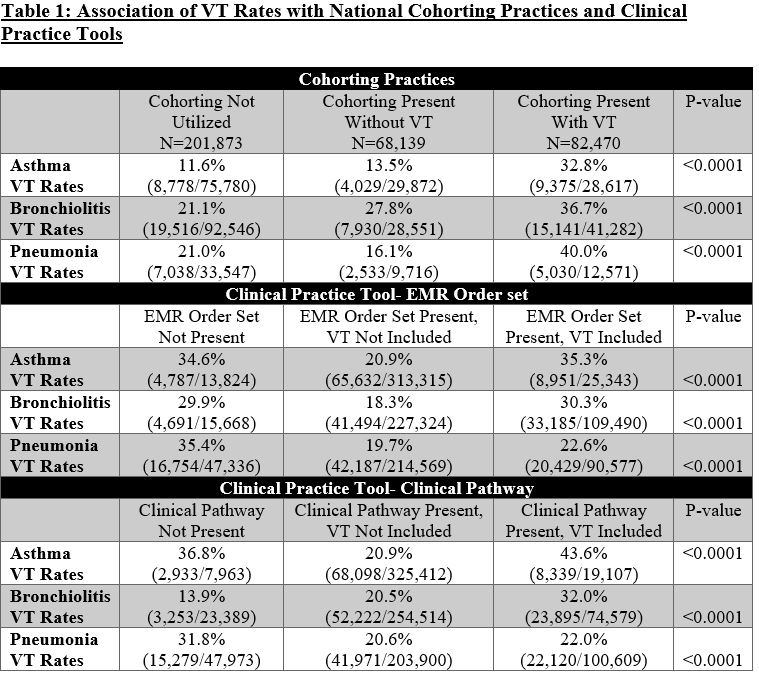
Results: Of the total 373,626 eligible patients, from 2014-2018, there were 142,517 patients with asthma, 171,844 patients with bronchiolitis, and 59,265 patients with pneumonia included in the study. Over the study period, during respiratory season, VT rates for asthma decreased from 23.9% to 19.2%, in bronchiolitis VT rates decreased from 33.5% to 25.2%, and in pneumonia VT rates decreased from 31.5% to 27.4% (p<0.0001). In non-respiratory season, VT rates were lower for asthma and pneumonia compared to respiratory season each year, however, VT rates were higher in non-respiratory season for bronchiolitis (Figure 1). 48 out of 52 PHIS hospitals responded to the survey (92% response rate). 44% (21/48) of PHIS hospitals utilize cohorting during high census season and 27% (13/48) specifically use VT for cohorting purposes. VT rates for PHIS hospitals who utilize VT for cohorting compared to hospitals who do not cohort were 32.8% vs 11.6 % (p<0.0001) in asthma, 36.7% vs 21.1% (p<0.0001) in bronchiolitis, and 40.0% vs 21.0% (p<0.0001) in pneumonia (Table 1). VT rates were lowest for each diagnosis in hospitals who had disease specific EMR order sets that did not include VT . In asthma and pneumonia, VT rates were lowest for hospitals who had a clinical pathway that did not include VT compared to hospitals who did not have a clinical pathway or had a clinical pathway that included VT (p<0.0001). In bronchiolitis, VT was lowest in hospitals who did not have a clinical pathway (p<0.0001) (Table 1).
Conclusions: Overall VT rates at PHIS hospitals has decreased in asthma, bronchiolitis, and pneumonia over the last five years and does vary slightly depending on season. VT rates are impacted by the presence of cohorting as well as the presence of EMR order sets and clinical pathways for each diagnosis.