Background: In the United States (US), obesity is associated with a high burden of morbidity and mortality, and its prevalence is increasing. A higher prevalence of obesity disproportionately impacts rural (vs. urban) areas and the Midwest and South (vs. West and Northeast) regions (1-2). In addition, obesity is linked with greater healthcare costs compared to patients without obesity (3). Sparse information on hospitalization trends for patients with obesity limits the development of targeted interventions. This study aimed to evaluate the hospitalization trends of obesity by region and urbanicity.
Methods: We used the largest publicly available all-payer inpatient dataset in the US, the National Inpatient Sample, available from the Agency for Healthcare Research and Quality, and studied 66.4 million adult hospitalizations from 2011 to 2021 (4). We conducted a multi-year cross-sectional analysis of hospitalizations with primary or secondary International Classification of Disease (ICD 9 and 10) codes for obesity. Obesity was defined as body-mass index (BMI) ≥30 kg/m2. We defined regions using the US Census Bureau system (4 regions: Northeast, Midwest, South, West). We characterized the urbanicity of patients’ residences at the county level using the 2013 National Center for Health Statistics system (3 categories: metro, medium-small, and rural). We compared patient characteristics and reported chi-squared (categorical) or Kruskal-Wallis (continuous) tests. We used multivariable linear regression to model obesity prevalence (per 100 hospitalized patients, adjusted for age and sex) and compared across regions.
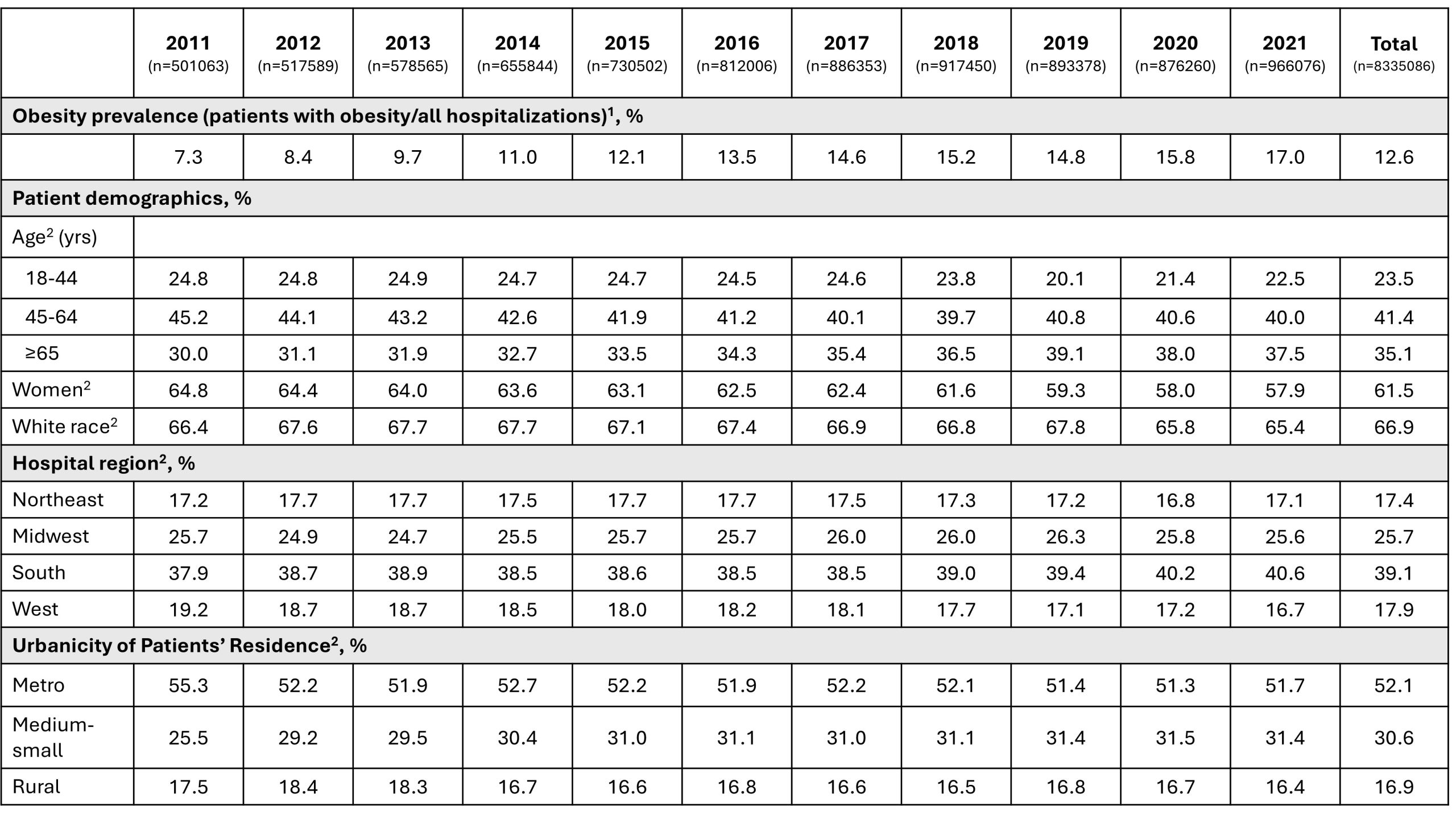
Results: Overall, from 2011–2021, 12.6% of hospitalized patients had obesity (n=8,335,086/66,394,666). Patients with obesity were more often women vs. men (61.5% vs. 38.5%; P <.0001) (Table). Among patients with obesity, the proportion of adults aged 18-44 years changed from 24.8% (2011) to 20.1% (2019) to 22.5% (2021), whereas adults aged 45-64 years showed an overall declining trend. Among patients with obesity, the proportion of patients of Black race declined (-1.0% total, P < .0001), and patients of Hispanic and Asian or Pacific Islander race increased (+1.5% and +0.4% total, respectively; P < .0001). The prevalence of hospitalized patients with obesity increased over time in all regions and urbanicity levels after adjusting for age and sex (Figure; p< 0.05). The Midwest had the highest prevalence in all urbanicity levels, while the Northeast and West tended to have the lowest prevalence in metro and rural areas, respectively. The change in prevalence was highest in the Midwest, increasing 1.9-fold from 2011 to 2021 in all rurality levels (p< 0.05). There was no statistically significant difference in the change in prevalence across regions (all, P≥.05).
Conclusions: In the US, from 2011–2021, the prevalence of obesity in hospitalized patients increased in all regions and urbanicity levels, with the largest and smallest magnitudes in the Midwest and West, respectively. To our knowledge, this is the largest analysis of US hospitalization trends in obesity. Further studies are required to evaluate hospital outcomes and sociodemographic drivers to inform regional interventions for obesity management.