Case Presentation: A 55-year-old woman with intravenous polysubstance abuse presented with a 1-week history of back pain, fever, and cough with blood-tinged sputum. Vital sign on admission showed tachycardia and hypotension but she responded well to fluid resuscitation. A pansystolic murmur grade 2 was noted. There was diffuse midline and paraspinal tenderness over the back.
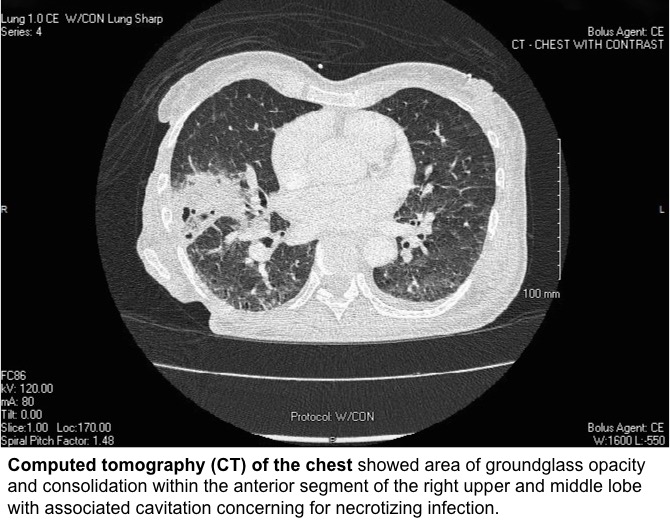
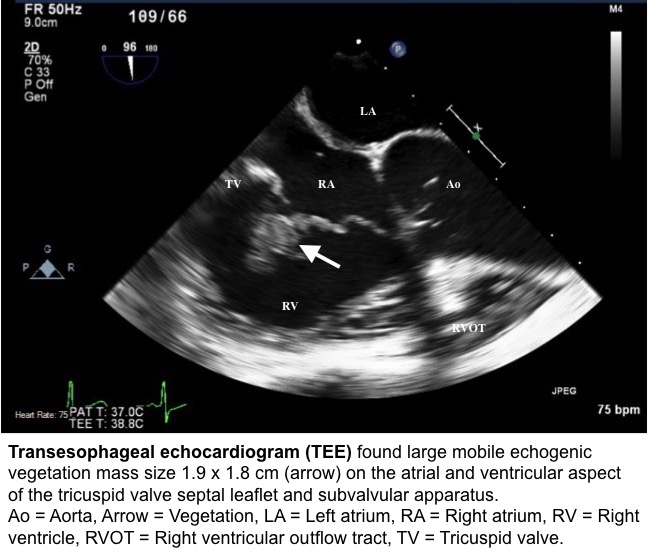
Blood tests were significant for leukocytosis with neutrophil 85.7%, elevated CRP and elevated ESR. She had negative HIV Ab/Ag test. Computed tomography (CT) of the chest revealed consolidation in the right middle lobe with cavitation concerning for necrotizing infection. Blood culture grew Klebsiella pneumoniae that was susceptible to ceftriaxone and was string test negative. Sputum culture grew 2 strains of Klebsiella pneumoniae, one with negative string test and the other with positive string test. Transesophageal echocardiogram found large mobile echogenic vegetation (1.9 x 1.8 cm) on tricuspid valve leaflet. MRI of the spine showed L4-5 discitis osteomyelitis with epidural and paraspinal abscess.
The patient underwent CT-guided paraspinal abscess drainage and tricuspid valve repair using tricuspid annuloplasty ring. The tricuspid vegetation showed 4+ WBC but no growth in culture. The patient completed 2 weeks of gentamicin and 6 weeks of ceftriaxone without recurrent endocarditis.
Discussion: Right-sided infective endocarditis (IE) is accounting for 5-10% of IE cases. However, it is strongly associated with intravenous drug use. Klebsiella pneumoniae is the second most common cause of gram-negative bloodstream infections. However, Klebsiella species caused only 1.2% of cases of native valve endocarditis. This low rate of IE may be related to its poor adherence of to cardiac valves.
Systemic embolism is a rare presentation of isolated tricuspid valve IE without co-existent left-sided vegetation, intracardiac right-to-left shunt, or intrapulmonary shunt. To determine hypervirulent Klebsiella pneumoniae (hvKP), the organism needs to meet at least 2 indicators: a positive string test, amplification of rmpA (regulator of mucoid phenotype A), and amplification of aerobactin. About 92.9% of hvKP has a positive string test; therefore, not all hvKP strains exhibit the hypermucovisity. The metastatic infection, as well as the presence of a string test positive strain in the sputum, raises suspicion of hvKP in our patient.
The most commonly used antibiotics for Klebsiella pneumoniae IE are aminoglycosides and cephalosporins with the optimal duration of 6-week course therapy. Non-operative management of tricuspid valve IE is associated with 7–11% in-hospital mortality. However, those statistics do not take hvKP into account. Indications for surgery include large vegetation (≥20 mm), septic pulmonary embolism, failed medical therapy, infected prosthetic valves. Early surgical intervention could avoid on-going leaflet tissue destruction and increase the likelihood of valve repair, which showed a protective effect against recurrent IE compare to valve replacement. Therefore, early tricuspid valve repair should be considered when possible.
Conclusions: Klebsiella pneumoniae is a rare but extremely dangerous cause of bacterial infective endocarditis. Systemic metastatic infection could occur in hypervirulent Klebsiella pneumoniae infection. Combined antibiotic and early surgical intervention are an optimal management for isolated tricuspid valve infective endocarditis due to Klebsiella pneumoniae.