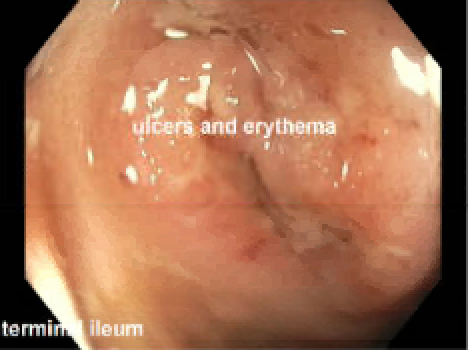
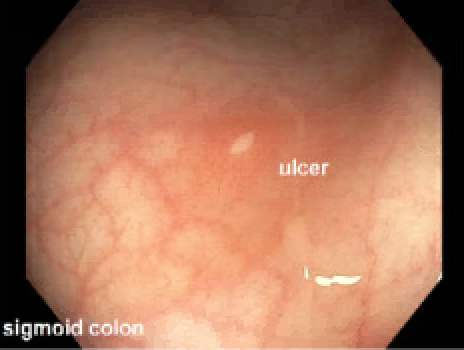
Case Presentation: A 4-year-old previously healthy boy presented with 10 days of fevers, intermittent abdominal pain, and poor appetite. Exam was notable for mild abdominal distension without tenderness. Labs showed leukocytosis, normocytic anemia, and elevated inflammatory markers. An echocardiogram showed mild dilation of his left anterior descending and left main coronary arteries, and he was treated for incomplete Kawasaki Disease with intravenous immunoglobulin and aspirin. He defervesced and had interval resolution of coronary ectasias on repeat echo. Within 24 hours of discharge, however, he was readmitted with recurrent fevers, two episodes of nonbloody diarrhea, and a self-resolving buccal ulcer, prompting further infectious and gastrointestinal workup. The infectious workup was negative despite daily fevers, but his fecal calprotectin was elevated to 1774 mg/kg (ref: 4 years old). Esophagogastroduodenoscopy (EGD) and colonoscopy were considered but deferred to the outpatient setting given the patient’s interval resolution of fever and poor bowel preparation tolerance. Six weeks later, he was readmitted with recurrent fevers and abdominal pain; of note, his weight had remained stable at the 97th percentile. EGD/colonoscopy revealed ulcers and erythema in the stomach, duodenum, terminal ileum and colon. The biopsy showed non-necrotizing granulomas, consistent with a diagnosis of Crohn’s disease or Very Early Onset Inflammatory Bowel Disease (VEO IBD). He was treated with exclusive enteral nutrition as induction therapy and infliximab as maintenance therapy, with complete resolution of symptoms.
Discussion: Fever of unknown origin (FUO) is a common condition for pediatric hospitalists to encounter, and most hospitalizations result in identifying an infectious etiology or without a diagnosis at all. IBD rarely presents as FUO, but should be considered in patients presenting with GI complaints after infectious etiologies are ruled out. While the reference range for fecal calprotectin is not well-established in young children, it is a sensitive marker for IBD and can be a helpful first step. Magnetic resonance elastography (MRE) or endoscopy should be considered if fecal calprotectin exceeds 250 mg/kg.The incidence of pediatric IBD in North America is approximately 26 per 100,000 and VEO IBD (onset before 6 years old) comprises 4-10%. The presentation of VEO IBD ranges from classic symptoms such as abdominal pain, weight loss, and diarrhea to more subtle changes such as growth failure and pubertal delay. Rectal bleeding is common, likely secondary to the colonic predominance in VEO IBD. Monogenic primary immunodeficiency, which manifests in 20% of VEO IBD cases, is often aggressive and refractory to standard therapies.Although VEO IBD can present with various symptoms, our patient only manifested FUO and mild GI symptoms despite severe pathologic findings on endoscopy. We postulate that his persistent fever may have been caused by bacterial translocation from his inflamed GI tract to his bloodstream, though no bacteria was ever isolated.
Conclusions: Fecal calprotectin may be a reasonable step in FUO evaluation, followed by MRE or endoscopy if significantly elevated. Although VEO IBD is a rare condition, clinicians should consider it in young children presenting with prolonged fever and a localized GI complaint after infectious etiologies are ruled out. Early diagnosis and prompt intervention can result in favorable prognosis.