Background: Tumor lysis syndrome (TLS) is a major life-threatening oncological emergency where accelerated damage of rapidly proliferating tumor cells results in critical metabolic derangements including hyperuricemia, hyperkalemia, hyperphosphatemia, and hypocalcemia potentially leading to acute kidney injury (AKI) and multi-organ failure. TLS has been well documented in hematologic malignancies but is extremely rare in solid neoplasms, particularly in prostate cancer. In this article, we investigate the clinical characteristics and outcomes of TLS in the available literature and our practice relevant to patients with prostate cancer.
Methods: We conducted a systematic review with a comprehensive literature search for published cases of TLS in prostate cancer. Statistical analysis of the pooled data from the literature search and cases identified at our institution were described.
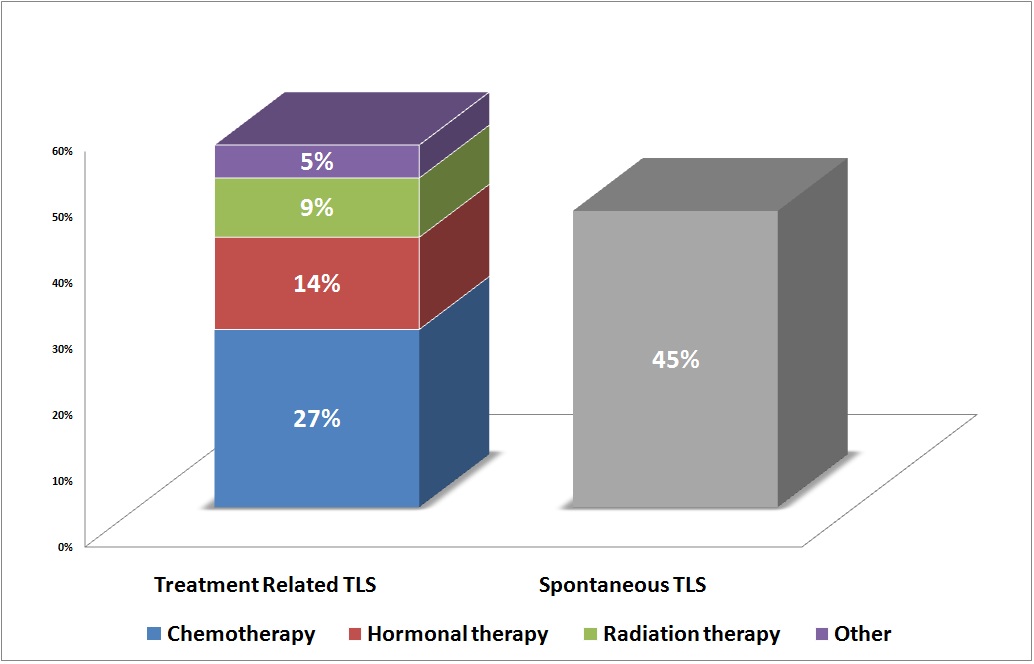
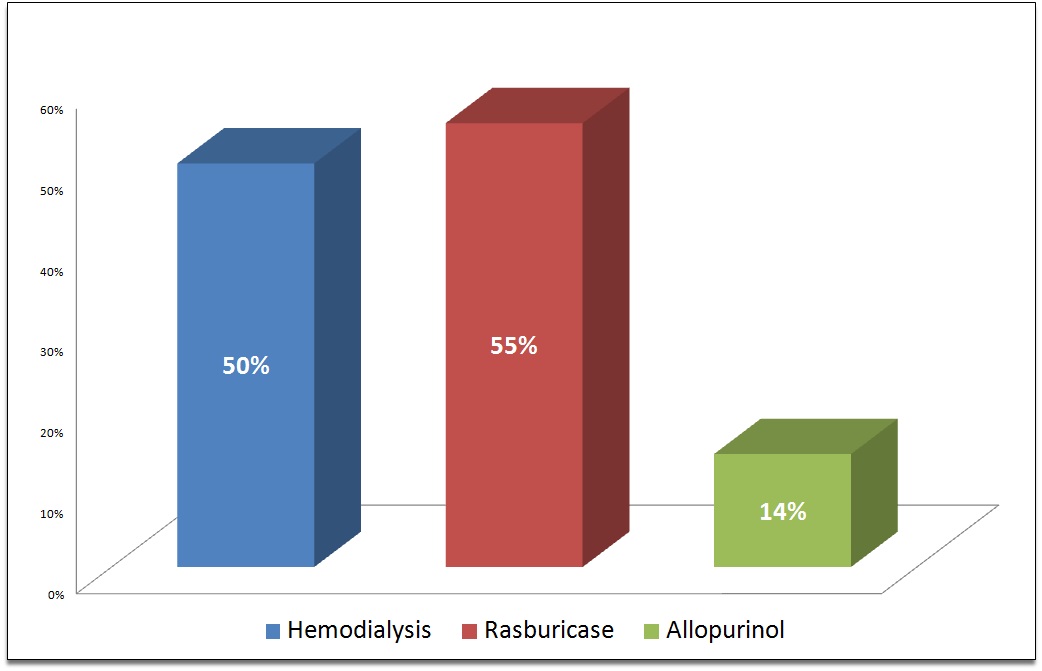
Results: We recognized 18 publications where TLS occurred in the setting of prostate cancer out of which 12 were treatment-related TLS and 6 happened spontaneously. Also, we identified four cases of spontaneous TLS diagnosed in our institutional database. The final cohort was consistent with a total of 22 prostate cancer patients with TLS. The median age of patients was 68 years and the median prostate-specific antigen was 374. The majority of cases were prostate adenocarcinoma (except one with prostate rhabdomyosarcoma, two cases with small cell prostate carcinoma, and four cases didn’t report the prostate cancer pathology type). TLS occurred as a consequence of cancer therapy in 55% of patients while 45% occurred spontaneously. Chemotherapy was associated with 27% of cases, hormonal therapy was complicated with TLS in 14% of cases, radiation therapy complicated 9% of cases. There was one reported case that developed TLS after treatment with methylprednisolone for pembrolizumab induced acute liver injury (5%). All patients had elevated LDH with other biochemical variables such as uric acid, potassium, phosphorus, and creatinine and all patients received aggressive supportive therapy. Metastasis is documented to the bone in 86.4% and viscera in 59.1% of TLS cases. Fifty percent of cases undergone hemodialysis. Rasburicase used in 55% of cases together with supportive therapy or in combination with hemodialysis and 14% of cases received allopurinol. The mortality rate was 75% among 12 cases of treatment-related TLS. The mortality rate was 30% in the ten patients with spontaneous TLS. No reported mortality in the 4 cases recognized and managed in our hospital.
Conclusions: This review highlights the life-threatening nature of TLS, a previously under-recognized complication of prostate cancer. The true incidence of TLS in solid tumors, particularly prostate cancer cases, still need attention as TLS can mimic AKI with metabolic abnormalities in its presentation. Currently, there is insufficient evidence to recommend one particular treatment over others when TLS is suspected. Physicians should be alerted to monitor for TLS. This review provides the most current information regarding the clinical features and outcome of TLS in prostate cancer for the development of optimal management strategies for this rare, but potentially fatal complication.