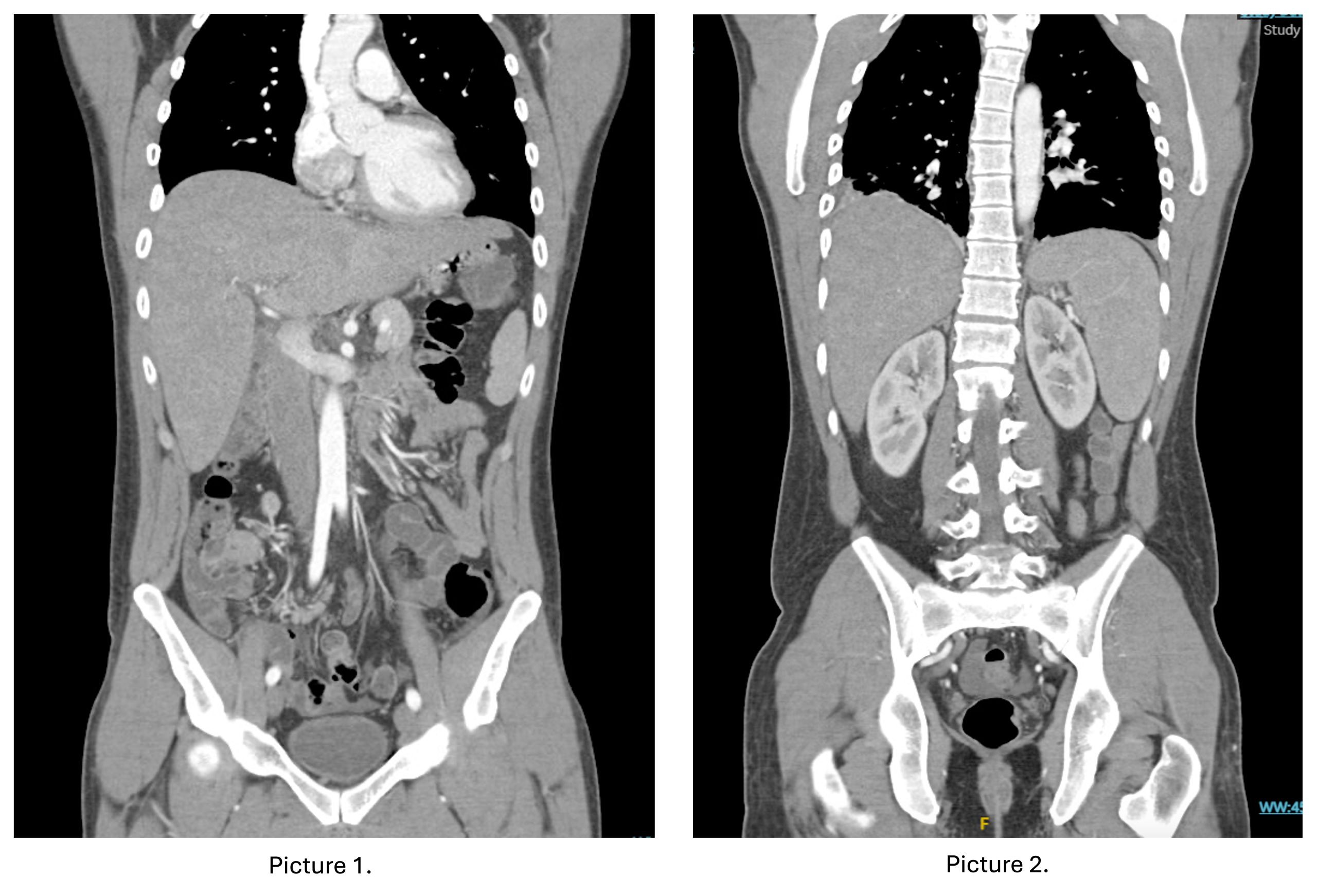
Case Presentation: A 30-year-old man with a remote history of Kawasaki disease and eosinophilic esophagitis, presented with 5 days of fevers, poor appetite, fatigue, and diarrhea after returning from India. Upon arrival, he was febrile (39.1°C), had a normal heart rate, and hepatosplenomegaly. Blood cultures demonstrated Salmonella Typhi, and stool polymerase chain reaction showed Salmonella species. Abdominal computed tomography showed enterocolitis, hepatosplenomegaly, and mesenteric lymphadenopathies. During hospitalization, he developed pancytopenia (WBC 3.9 x 10³/uL, hemoglobin 11.7 g/dL, platelets 102 x 10³/uL) with signs of hemolysis (haptoglobin < 8 mg/dL, LDH 1310 U/L), transaminitis (ALT 77 IU/L, AST 110 IU/L), and acute kidney injury (creatinine 1.5 mg/dL). He was treated with ceftriaxone for Salmonella bacteremia. His hospital course was notable for worsening transaminitis (ALT 894 IU/L, AST 1188 IU/L), ultimately thought to be secondary to Salmonella hepatitis. A 14-day course of sulfamethoxazole/trimethoprim was recommended. The patient had improved transaminitis and kidney injury on discharge, with plans to follow up as an outpatient.
Discussion: Salmonella enterica spp. are gram-negative, rod-shaped bacteria in the Enterobacteriaceae family that are prevalent in Latin America, Africa, and Asia. Typhoidal serovars (Typhi and Paratyphi) can cause disseminated disease in immunocompetent hosts, with incubation periods of 7 to 21 days, and symptoms lasting up to 3 weeks [2]. In addition to causing diarrhea via local inflammation, these bacteria can enter the lymphatic system through M cells in Peyer’s patches, and then live and replicate intracellularly within the reticuloendothelial system causing extraintestinal manifestations such as hepatosplenomegaly, and bone marrow failure [3]. Typhoidal serovars can also cause hemolysis through hemolysins [4]. This patient had enteric fever due to Salmonella enterica serovar Typhi infection. The CDC estimates that 620 people are hospitalized per year in the United States for this condition, and most of the cases are in international travelers. As often described, the patient had relative bradycardia, mesenteric lymphadenopathies, and hepatosplenomegaly, which reflect the infiltration of the reticuloendothelial system. Remarkably, he also presented with hemolysis and hepatitis, both infrequent complications. Despite hemolysis having been classically described, it has not been frequently reported in the literature, except for one case report in 2024 [4]. The process is mediated by the release of hemolysin E, which is triggered by the presence of stress hormones, and usually presents within the first 14 days of infection [5]. Mild liver test abnormalities can be seen in salmonellosis; however, severe hepatitis is uncommon and may mimic viral hepatitis. The pathogenesis is multifactorial and can be caused by direct damage from endotoxins and a combination of local inflammation and the host’s immune response. When severe, the mortality can be up to 20%, but it typically responds favorably to antibiotic [6].
Conclusions: This case highlights the diverse complications of enteric fever, which remains a rare cause of hospitalization in the United States, underscoring the importance of considering this diagnosis in patients who have traveled to endemic areas, and who present with prolonged fevers and systemic symptoms such as hepatitis or hemolysis.