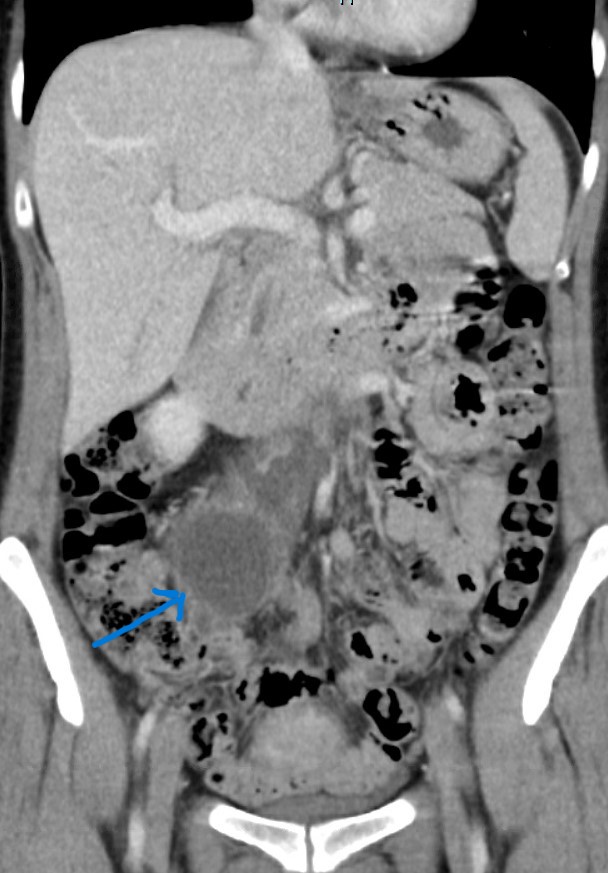
Case Presentation: We present a case of a 42-year-old woman admitted to the ICU for management of suspected septic shock. She presented with right lower quadrant and back pain for the past day, fever, nausea, and vomiting. Her blood pressure was 70/46 mm of Hg and examination was significant for right lower abdominal quadrant tenderness. Significant laboratory findings were a white blood cell count of 27000 per µL, procalcitonin 22 ng/mL, lactic acid 1.1 mmol/L, normal urine analysis, negative beta-hCG, and blood culture positive for streptococcus agalactiae. CT scan abdomen and pelvis revealed thick-walled fluid collection (6cm x 3.5cm x 5.7cm) in the right retroperitoneum anterior to the psoas muscle. It had simple fluid density not compatible with acute hemorrhage representing lymphatic malformations. There was also free fluid in the retroperitoneum from the leaking of the cysts. There were several retroperitoneal cysts, a cyst on the left kidney (2.3 cms), and bilateral adnexal cysts with possible abscess. HRCT scan of the lung revealed diffuse cystic lung disease (cysts measuring up to 13 mm) consistent with the diagnosis of LAM, bilateral pleural effusions, suggesting possible chylous effusions. VEGF-D was found to be 1040 pg/ml. Broad-spectrum antibiotics, fluid resuscitation and norepinephrine drip was started. After she recovered from the septic shock, outpatient follow-up was scheduled for this newly diagnosed LAM syndrome
Discussion: Lymphangioleiomyomatosis (LAM) is a rare syndrome that predominantly affects women of reproductive age (3.4–7.8 per million women worldwide) and 66% of patients at presentation are usually in their 3rd-4th decade of life(1). There is formation of fluid-filled cysts in axial lymphatics and thin-walled cysts in bilateral lungs by LAM cells which cause the destruction of the lung parenchyma(2). There are two types of LAM syndrome: one caused by mutation of TSC-2 genes occurring sporadically and another in association with tuberous sclerosis complex (TSC) caused by mutation of TSC-1 or TSC-2 genes. There is proliferation of LAM cells which have characteristics of smooth muscle and melanocytes because of the activation of the mechanistic target of rapamycin signaling pathway(1). Most commonly present with pulmonary symptoms like recurrent pneumothorax (risk is 1000 times more than the general population), chylous pleural effusions or dyspnea(4). Other clinical features include renal angiomyolipoma, chylous ascites, hemoptysis, lymphatic fluid-filled retroperitoneal cysts(5). Our patient did not have a history of any respiratory symptoms. She presented with septic shock secondary to one of the retroperitoneal cysts becoming secondarily infected. For diagnosis, HRCT findings and either one of the following are required: renal angiomyolipoma, VEGF-D level >800 pg/ml, lymphangioleiomyomas, or thoracic/abdominal chylous effusions(1). Differential diagnosis of diffuse cystic lung disease includes Sjogren’s syndrome, pulmonary Langerhans cell histiocytosis, emphysema, follicular bronchiolitis, lymphoid interstitial pneumonia, and Birt-Hogg-Dubé syndrome (5). Sirolimus and everolimus are approved by FDA from LAM syndrome(3). Other ongoing research trials include a combination of sirolimus with either simvastatin, hydroxychloroquine, or resveratrol(3)(5).
Conclusions: We are reporting an unusual complication arising from this rare syndrome which have not been documented so far and importance of finding out the cause of the presenting complaint.