Background:
Whether an unplanned intensive care unit transfer (UICUT) results from an error in care and whether these transfers can be prevented has not been previously investigated. We sought to determine the causes of UlCUTs of patients to a medical ICU, whether they resulted from errors in care, and when clinical deterioration was noted, whether an earlier or different response might have prevented such transfers.
Methods:
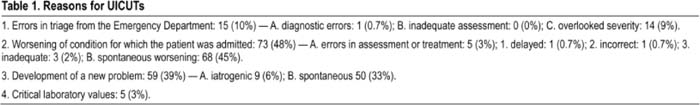
This was a single‐center observational cohort study of all patients between 18 and 89 years of age with UlCUTs over a period of 1 year from July 2005 to June 2006. Exclusion criteria included patients transferring from outside hospitals or from non‐Medicine units, direct admissions to the ICU. readmissions to the ICU, planned transfers following invasive procedures, and patients who were pregnant or prisoners. We recorded demographics, admission and transfer diagnoses, reasons for unplanned ICU transfers based on a defined taxonomy (Table 1). presence of signs of clinical deterioration, mortality, judgment by 3 independent reviewers about the causes of the ICU transfer, and whether it could have been prevented. Associations between baseline and outcome variables were assessed using the X2 test. Agreement between the reviewers was assessed using the k statistic
Results:
One hundred and fifty‐two patients met the study criteria. The most common diagnoses for a UICUT were respiratory failure (24%) and acute coronary syndrome (11%). The reasons for UlCUTs are listed in Table 1. Mortality was lower for patients when the transfer occurred within 24 hours of admission (4% versus 22% mortality if transfer was < 24 versus > 24 hours after admission, 0.29, P < 0.05, 95% CI 0.09–0.89). Errors in care accounted for the transfer in 29 patients (19%), but in 15 of 29 patients (52%) the errors were in triage as 14 of 15 (93%) met ICU admission criteria while still in the emergency department. One hundred and six patients (70%) had 1 or more signs of clinical deterioration within the 12 hours preceding the ICU transfer. For these patients, all 3 reviewers agreed and concluded that 94 of 109 patients (89%) even with a different or earlier intervention would still have needed a transfer to the ICU. Interobserver reliability for the 3 reviewers was good, with k = 0.60 (95% Cl 0.33, 0.87); k = 0.82 (95% Cl 0.59,1.05); and k = 0.63 (95% Cl 0.36, 0.88).
Conclusions:
Examining the causes of UlCUTs revealed a target for improving the quality of care in our institution. As many as 19% of such transfers were potentially preventable. Our data do not support the use of rapid response teams to reduce UlCUTs.
Author Disclosure:
S.Bapoje, none; J. Gaudiani, none; V. Narayanan, none; R. Albert, none.