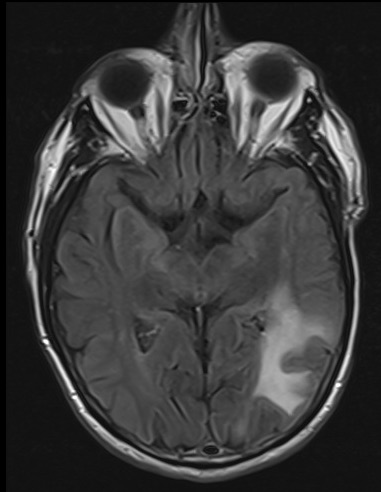
Case Presentation: A 73 year-old man presented with 2 weeks of difficulty completing multi-step tasks, e.g., getting into a car. At baseline, he was independent in instrumental activities of daily living. He had no other symptoms; he denied headache, weakness, numbness, vision changes, confusion, fevers, chills or weight loss. His history included non-alcoholic steatohepatitis with cirrhosis complicated by portal hypertension and hepatocellular carcinoma for which he had received 2 radioembolizations with Yttrium-90. He never received systemic chemo- or immunotherapy. He was oriented to person, place and situation but reported the year as “20-0-2” (the year was 2022). He was not jaundiced and did not have asterixis. He had mild deficits in word-finding, calculation and attention. He followed 1- but not 2-step commands. Naming, speech and repetition were intact, and cranial nerve, sensory, motor and cerebellar exams were normal. Liver function tests and white cell count were within normal limits. Serum ammonia was 76 mcg/dL. Computed tomography head scan revealed 2 discrete areas of vasogenic edema in the bilateral parietal lobes. Brain magnetic resonance imaging (MRI) revealed non-enhancing lesions in bilateral parietal and left occipitotemporal lobes concerning for an inflammatory or demyelinating process with no space-occupying component. Cerebrospinal fluid (CSF) chemistry and cell counts were normal; oligoclonal bands and malignant cells were absent. CSF BioFire assay for meningitis and encephalitis pathogens was negative. Serum tests for Epstein Barr virus, cytomegalovirus, and human immunodeficiency virus (HIV) and blood cultures were also negative. He received lactulose and high-dose intravenous steroids without improvement in neurologic exam. Brain biopsy was deferred, and he was discharged. Four days later, he returned with a rapid decline in neurologic status, disoriented and unable to complete activities of daily living. Serum JC virus antibody assay had returned positive in the interim. Repeat brain MRI revealed increased size and extent of the non-enhancing white matter lesions noted previously. Repeat CSF analysis revealed a positive CSF JC virus PCR assay, confirming diagnosis of progressive multifocal leukoencephalopathy (PML). The patient’s mental status rapidly declined, and he died 6 weeks after initial symptom onset.
Discussion: PML is a rare disease that disrupts the cerebral white matter due to cell-mediated immunosuppression resulting in opportunistic neurotropic JC virus infection of glial cells. Neurologic presentation is variable given the non-uniform infection with JC virus. Diagnosis is confirmed with JC virus in the CSF and representative imaging (multifocal white matter demyelination) or a brain biopsy consistent with PML histopathology. The most common immunosuppressive states associated with PML are HIV, immunosuppressive therapies, blood cancers, inherited immunodeficiencies and rheumatologic diseases; those without HIV have shorter median survival.
Conclusions: Though uncommon, cirrhosis has been linked to PML in a case series of 7 patients. The proposed immunosuppressive mechanism in cirrhosis is hypogammaglobulinemia and relative leukopenia from white cell splenic sequestration in portal hypertension. In patients with cirrhosis who present with focal neurologic changes and demyelinating brain lesions, hospitalists should include PML on the differential.