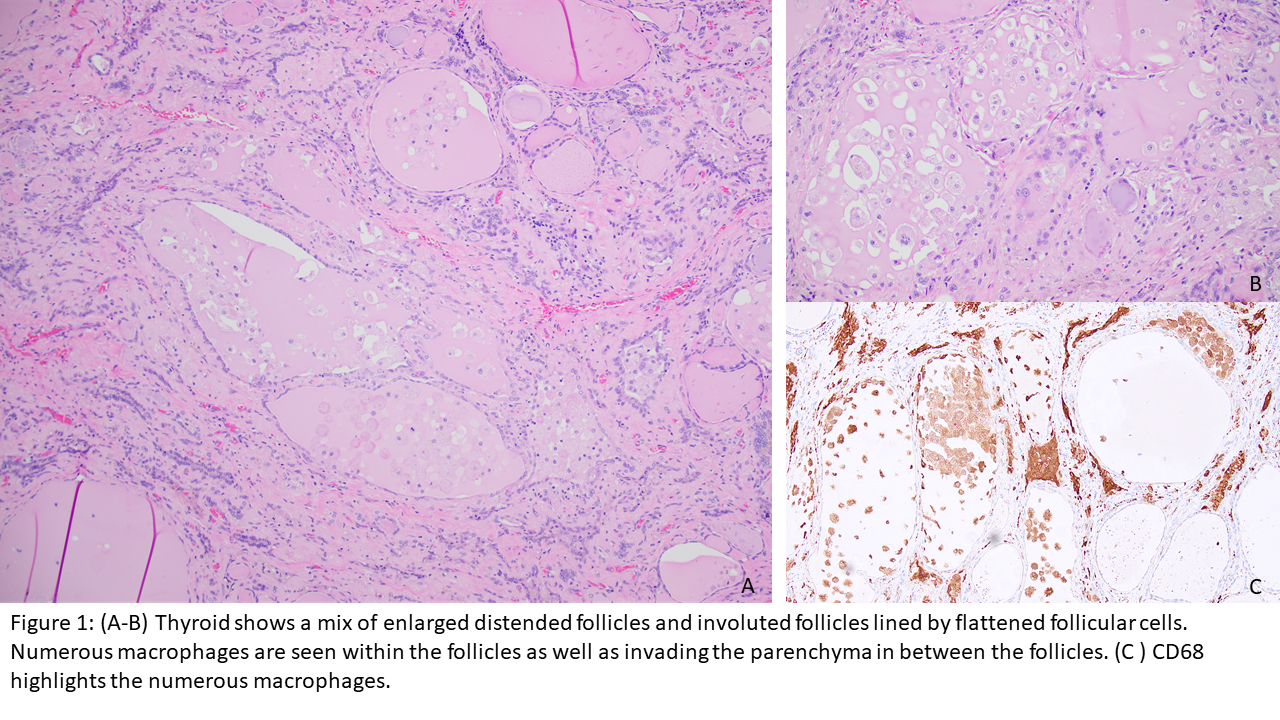
Case Presentation: A 60-year-old male with a history of diabetes, chronic kidney disease, and ventricular tachycardia treated with amiodarone for three total years prior to orthotopic heart transplant one year ago was admitted to the hospital for abdominal pain. He was diagnosed with cholecystitis and underwent uncomplicated laparoscopic cholecystectomy. The postoperative hospital course was complicated by restlessness and hyperactive delirium. During admission, the patient had disorientation, periodic hallucinations, restlessness, weakness, confusion, anxiety, difficulty sleeping, cold intolerance, and intermittent tremors. He remained hemodynamically stable with a pulse in the low 60s. CT of the head revealed chronic ischemic microvascular changes. Neurology was consulted with subsequent workup negative for prion disease, paraneoplastic encephalitis, and epilepsy. Psychiatry was also consulted for management of hyperactive delirium. Finally, thyroid workup revealed elevated free T4 and T3, with reduced thyroid-stimulating hormone (TSH). Thyroid-stimulating immunoglobulins and thyroid receptor antibodies were negative. Despite methimazole, hydrocortisone, and propranolol, his free T4 levels remained persistently elevated prompting a total thyroidectomy. Histopathologic thyroid examination supported a diagnosis of type 1 amiodarone-induced thyrotoxicosis, which was further supported by prior exposure to amiodarone for 3 years.Following total thyroidectomy, the patient’s altered mental status slowly improved with normalization of free T4 and improving TSH. Subsequently, he was started on levothyroxine replacement. Throughout the hospital stay, there were no documented episodes of tachycardia, arrhythmia, or hemodynamic instability. He was discharged fully alert and oriented to person, place, and time.
Discussion: Thyrotoxicosis occurs in approximately 6–13 % of patients taking amiodarone, depending upon dietary iodine intake. Thyrotoxicosis presents as a multi-system illness with clinical picture dominated by perturbation of the cardiovascular system that may manifest as tachycardia, increased cardiac output, heart failure, or atrial fibrillation. Narrowing the differential diagnosis to persistent thyrotoxicosis was difficult given the predominant central nervous system involvement on initial presentation. The absence of cardiovascular symptoms was most likely due to denervation of the recently transplanted heart which yielded resistance to actions of thyroid hormones that are predominantly manifested through adrenergic receptors. In this case, thyrotoxicosis was the most likely diagnosis due to lack of an alternative medical explanation and improvement of neuropsychiatric status congruent with normalization of thyroid levels. To our knowledge, there have been very few reported cases of post-heart transplant thyrotoxicosis manifesting with isolated altered mental status (AMS).
Conclusions: This case highlights important considerations for clinicians. First, the importance of clinical, pathologic, and laboratory correlation to secure the correct diagnosis. Further, the role of multidisciplinary management for symptomatic management, appropriate diagnostic workup, and generation of a broad differential diagnosis in patients with AMS. Lastly, thyrotoxicosis must remain on the differential diagnosis for isolated AMS in patients with history of heart transplant in both the preoperative and postoperative thyroidectomy course.