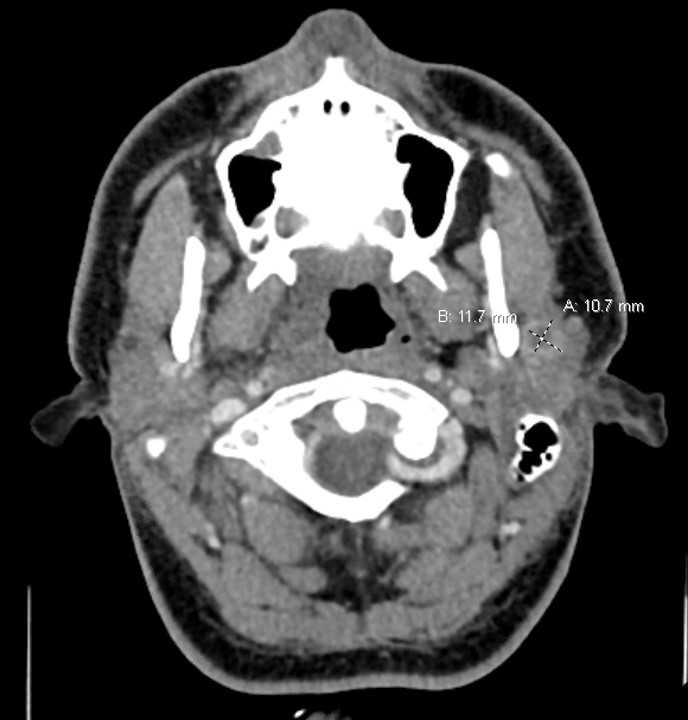
Case Presentation: A 25-year-old male without medical history presented with right sided throat pain, fever and chills for 3 days. He also had a painful swelling behind his left ear for 4 weeks. In the emergency department, examination showed an erythematous and edematous right tonsil with local mass effect on the uvula with left-sided displacement and a 3 cm x 3 cm raised fluctuance with overlying erythema in the L posterior auricular area. Computed tomography of the neck (CT) with intravenous contrast showed a right peritonsillar enhancing density (2.7 cm x 0.9 cm x 2.0 cm) and multiple fluid collections within the left parotid gland (Fig.1). He was admitted and treated with intravenous Clindamycin. Incision and drainage of the left postauricular and right peritonsillar abscesses released 15 ml and 20 ml of purulence, respectively. Specimen gram stain showed multiple polymorphonuclear cells. Abscess culture was no growth as well as blood cultures. He completed 7 days of Clindamycin with resolution of the pain and swelling in his neck area.Eight weeks later, he returned to his medical provider with a new left preauricular swelling and trismus. Repeat neck CT with IV contrast showed (Fig. 2) a complex, multiloculated peripherally enhancing collection centered within the superficial lobe of the left parotid gland. On further history, he revealed that he had 4 cats for years. Additional work-up revealed Bartonella henselae IgG titer of 1:512. He underwent surgical incision and drainage of the left parotid abscess which yielded thick yellow mucoid purulence. Routine microbiology studies again were negative. Specimen was sent for DNA sequencing and was positive for Bartonella henselae DNA. He completed 14 days of Doxycycline and had no recurrence of the infection on follow-up visits.
Discussion: Parotid abscess is a rare manifestation of cat scratch disease (CSD). It is often overlooked or misdiagnosed as a possible diagnosis especially if appropriate questions regarding exposure are not sought. There have been no case reports to date published of peritonsillar abscess from CSD (1-5). It is possible that this case’s peritonsillar abscess was also caused by Bartonella henselae. Cat scratch disease is typically diagnosed clinically if there is a classical presentation of a tender lymphadenopathy with or without an inoculation site in the setting of cat exposure. Diagnoses may be supplemented by Bartonella serologies or DNA sequencing from an appropriate specimen. Bartonella IgG titers ≥1:256 strongly suggest active or recent infection. Azithromycin, Rifampin, Trimethoprim-Sulfamethoxazole and Doxycycline are all active against Bartonella henselae. Our case highlights the significance of a thorough history taking especially in infectious syndromes.
Conclusions: This case emphasizes keeping CSD in the differentials if the usual predisposing conditions and precipitating factors are not identified in the history taking of someone presenting with a parotid abscess. If a patient is febrile with hemodynamic instability, hospitalization, initiation of empiric antibiotics therapy for sepsis and further work-up would have been appropriate but would still miss out on the potential diagnosis if pertinent history is not obtained. Source-control with incision and drainage are also appropriate but without the knowledge of a potential pathogen, key studies to reveal the diagnosis might be left out.