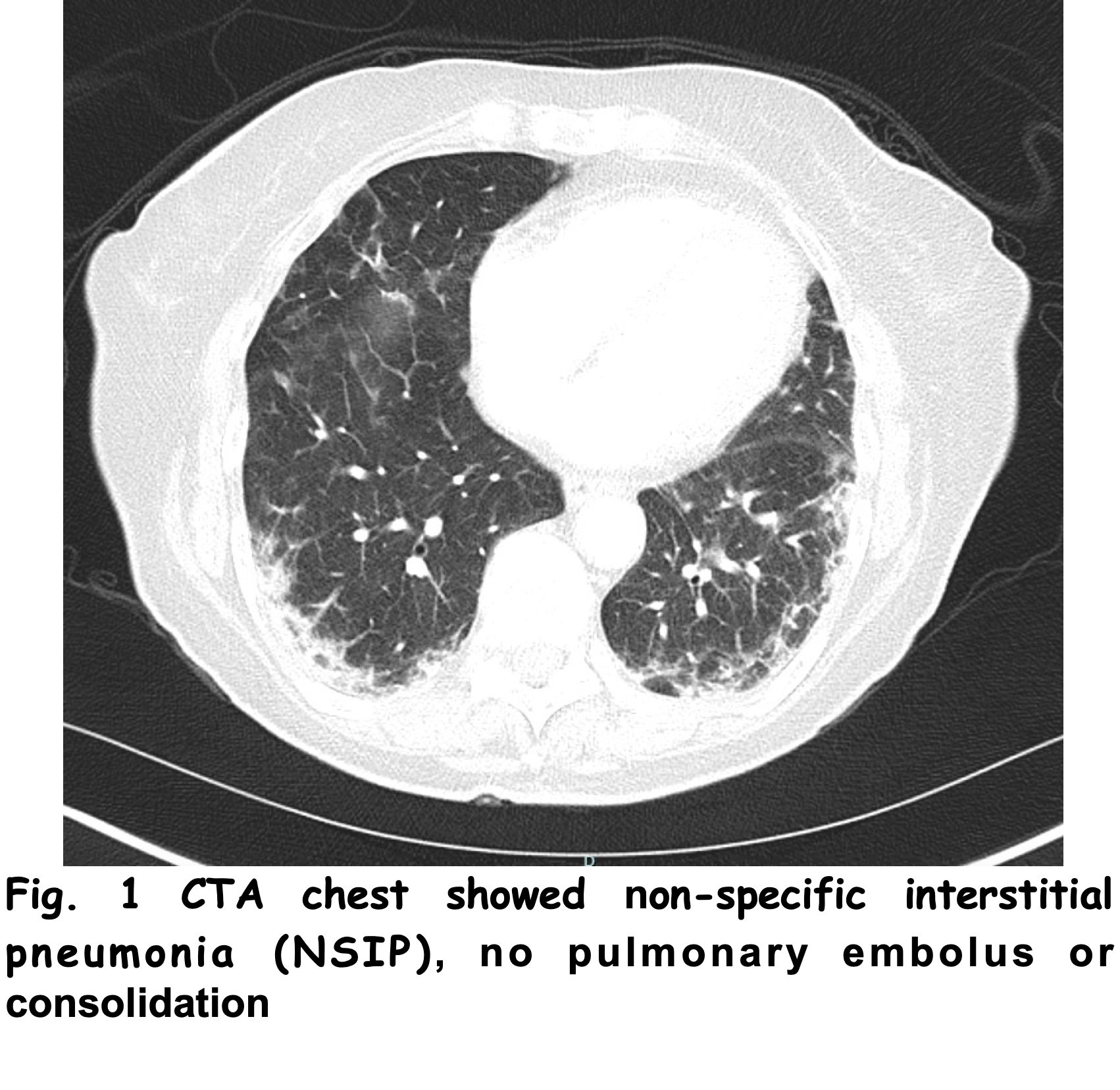
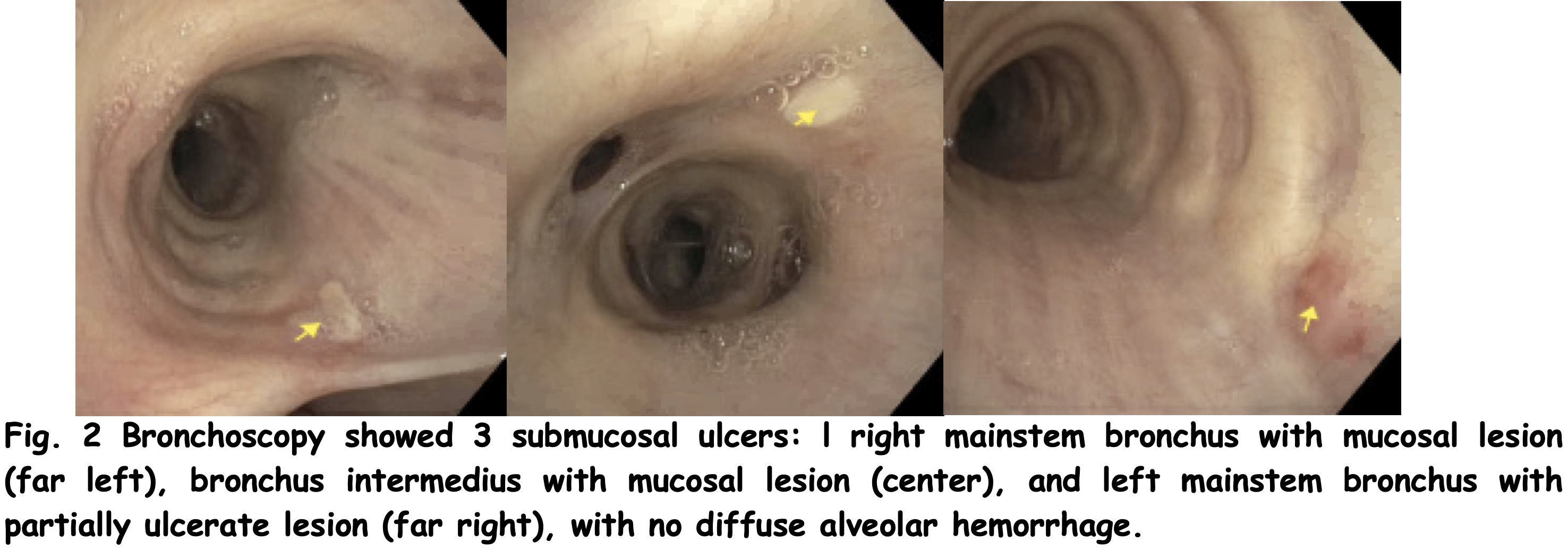
Case Presentation: A 70-year-old Caucasian woman with history of hypertension, hyperlipidemia, and newly diagnosed atrial fibrillation presented with persistent exertional dyspnea, fatigue, malaise, and anorexia for the past few days. She was recently discharged for community-acquired pneumonia twice at another institution without improvement of nonproductive cough, mild proximal muscle weakness, and exertional dyspnea. She was on prednisone 10mg daily and had completed dupilumab prior to admission for a nonspecific rash on the abdomen, which was biopsied and diagnosed as DRESS syndrome from valsartan.Physical examination showed afebrile, tachypneic to 24, with resting oxygen saturation of 100% on room air, but with exertion desaturated to 85%. Lung auscultation revealed scattered fine rhonchi and wheezes. Skin examination was notable for lip ulcerations. EKG showed atrial fibrillation. Chest X-ray showed bilateral interstitial and slight alveolar opacification, especially in lower lung fields. CTA chest demonstrated peripheral ground-glass density and interstitial thickening, but no pulmonary embolus. She was started on IV ceftriaxone, doxycycline, inhalers, lopressor, and anticoagulation. After third day of admission, patient still reported exertional dyspnea. Extensive infectious work-up, including 3 covid tests, was negative. Repeat pro-BNP increased to 1,348 pg/ml with persistent diffuse bilateral lung opacities on CXR. CK and ESR were normal, but CRP was elevated to 6.4mg/dL. IV fluids and antibiotics were stopped and she received IV furosemide and methylprednisolone. Echocardiography was normal. Bronchoscopy showed three bronchial submucosal ulcers without diffuse alveolar hemorrhage. BAL cytology, eosinophils, AFB, HSV, and fungal cultures were negative. Endobronchial biopsy revealed dysplasia of squamous epithelium, but without definitive evidence of malignancy. Patient was transiently on high-flow oxygen and weaned to 4L/min. Extensive rheumatologic workup yielded negative results except for elevated anti-SSA with mild elevation in aldolase(13 U/L), and low complement levels (C3,78mg/dL; C4,11mg/dL). She received Methylprednisolone 250mg every 12 hours for 5 days for presumed idiopathic pulmonary fibrosis with autoimmune features and was discharged home on prednisone 40mg daily. After hospital discharge, anti-MDA-5 antibody from myomarker3 panel returned positive. Repeat high resolution of chest revealed nonspecific interstitial pneumonia (NSIP). Patient was given rituximab 1000mg IV for presumed MDA-5 myositis.
Discussion: Cutaneous ulcers are identified in one-fourth of dermatomyositis (DM) patients and occasionally, characteristic cutaneous ulcers are strongly associated with specific autoantibodies, such as oral ulcers with anti-melanoma differentiation-associated gene5 product(MDA5) antibody. Here we describe a case of ulcers in an unusual location, as a potential clue for the diagnosis of anti-MDA-5 amyopathic dermatomyositis.
Conclusions: Few studies reported mucosal involvement of pharynx, larynx, and conjunctiva in DM patients. Few case reports discuss bronchial ulcers in DM patients. Starting steroids before establishing a diagnosis can delay diagnosis, and mask important physical exam findings such as characteristic rashes. Keeping a broad differential, and considering rheumatic disease is essential when evaluating patients with progressive exertional dyspnea unresponsive to antibiotics and a history of cutaneous rash.