Background: Anticoagulants are among the highest-risk medications in hospitalized patients. Studies have demonstrated that a majority of in-hospital anticoagulant adverse drug events are not only preventable, but are the result of excessive dosing. This is especially true for warfarin dosing, which is complicated by a lack of consensus among validated initial dosing nomograms. As part of a health system-wide anticoagulation group, we have introduced a warfarin safety initiative at a large tertiary care center that consists of two components: dose-capping in older adults and delta INR-based provider dosing education.
Purpose: To describe a dose-capping and delta INR project at a large tertiary, academic medical center and present initial findings.
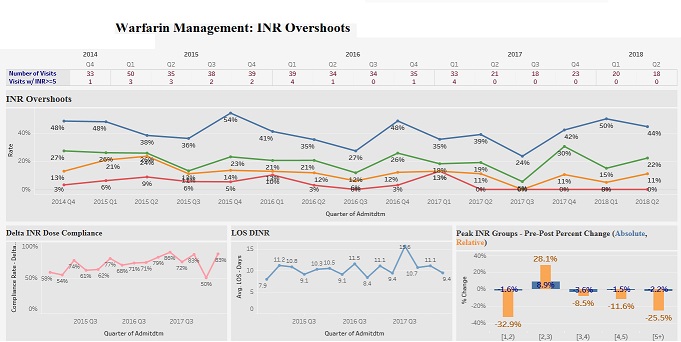
Description: Based on pilot projects at smaller community medical centers within our health system, we organized a multidisciplinary team including personnel from Hospital Medicine, Pharmacy, Administration, and Data Analytics. A graphical web-based dashboard was created for monitoring inpatients prescribed warfarin. This allowed team members to view individual patient INRs and warfarin doses, as well as the proportion of patients with INRs above various cutoff values (3.0, 3.5, 4.0, 4.5, and 5.0). Pharmacy team members screened the dashboard daily to identify patients at risk for adverse drug events and contacted providers directly with dosing suggestions. For patients age 85 and over, a capped first dose of ≤ 2.5mg daily was suggested. For patients with delta INR (i.e., the increase in INR value over the preceding 24 hours) ≥ 0.5, a patient-specific dose reduction was suggested; the dashboard included data on provider adherence with dose-capping and delta INR-based dose reduction suggestions.
Thus far, there has been 100% provider adherence with dose-capping recommendations for patients ≥ 85 years. In the last calendar quarter, the rate of INR > 3.0 in this cohort has decreased from 37% to 21%. For patients with delta INR ≥ 0.5, providers either decreased or held warfarin doses prior to pharmacist intervention in 71.4% of cases. In the remaining 28.6% of cases, a pharmacist made a dose recommendation; providers accepted dosing recommendations in 87.5% of these cases. During the last calendar quarter, the rate of INR > 3.0 in this cohort decreased from 41% to 33%. During this time period there has only been one case of INR > 5.0 in all studied patients. Moreover, length of stay (LOS) did not increase in either cohort.
Conclusions: A multidisciplinary program to monitor warfarin dosing via a web-based dashboard and follow-up with providers for intervention in near-real-time results in fewer supratherapeutic INRs in a high warfarin sensitivity population. Providers are generally accepting of Pharmacy dosing recommendations. The program showed initial success at a large, academic tertiary center without significantly altering typical workflow or consuming excess resources, and without apparently impacting LOS.