Background:
Strong physician communication skills can enhance the patient experience and improve patient satisfaction but data consistently reveal dissatisfaction with physician‐patient interactions with little evidence examining specific deficiencies among physicians. Further, few communication improvement strategies have been developed and tested. In order to improve communication and patient satisfaction, we developed a Standardized Patient (SP) program to identify deficits and provide feedback to our hospitalists.
Methods:
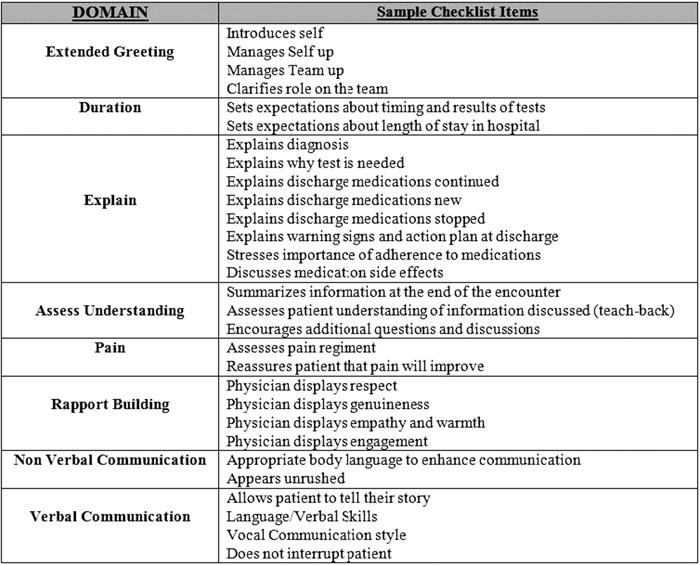
Our program consisted of three SP cases developed around common hospitalist‐patient interactions: daily rounding, discharge, and a difficult patient. For each case, we developed a structured checklist consisting of core elements for effective communication and patient satisfaction. Before each case, hospitalists were given pertinent clinical background and communication tasks. After each case, the SP and hospitalist watched a video of their encounter, and using the checklist, the SP gave the hospitalist feedback. The SPs scored each checklist item as inadequate, partial, or adequate. We grouped checklist items into the following domains: “extended greeting”, “duration”, “explain”, “assess understanding”, “pain”, “verbal communication”, “non‐verbal communication”, and “rapport building” (Table 1). We compared domains within each case and across cases. HCAHPS patient satisfaction scores were measured at baseline and 6 months after the intervention.
Results:
23 hospitalists participated in all three encounters. For the daily rounding case, hospitalists’ weakest domains were “duration” (p<.05) and “assess understanding” (p<.05) and in the discharge case, our hospitalists’ weakest domains were “assess understanding” (p<.05). For the difficult patient case, there were no significant differences across domains. When comparing across cases, hospitalists performed significantly better in the domain “extended greeting” (p<.05) and “assess understanding” (p<.05) for the difficult patient. Hospitalists performed significantly worse in the “explain” (p<.05) domain for the patient being discharged. There was no significant change in the HCAHPS score before and after the intervention.
Conclusions:
Using a novel SP exercise for hospitalists, we found that hospitalists’ weakest communication areas were assessing patient understanding of their medical care and explaining information. However, when hospitalists were challenged with a difficult patient, they were better at assessing patient understanding of their medical care, clarifying their role on the team, and managing up. Though the SP intervention did not improve HCAHPS scores, the results have allowed us to develop additional educational initiatives that target the identified weaknesses.