Background: Asthma is the leading chronic disease in children with prevalence approaching 10%. Barriers to follow up care, poor access to medication and lack of disease education pose a threat to patient safety and increase the risk for hospital re-utilization. The Improving Pediatric Patient Centered Care Transitions (IMPACT) collaborative designed and implemented a 4- element bundle (transition checklist, teach back, timely and complete communication with outpatient providers, and post-discharge phone call) with the aim of improving the hospital to home transition as evidenced by reduction of 30-day readmissions (RR). The purpose of this study was to identify the effect of individual or combined bundle element on reducing 30-day RR for asthma patients.
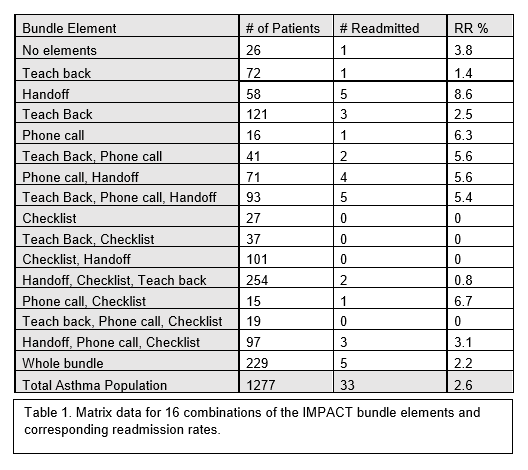
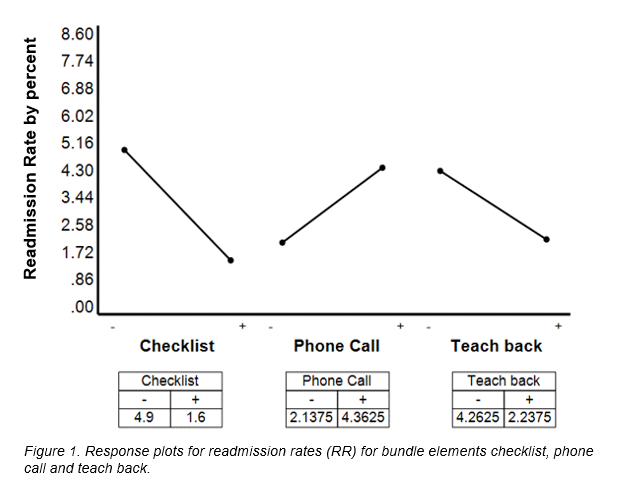
Methods: This was a retrospective analysis of individual asthma patient readmission and bundle element exposure collected from January 2014 to December 2017. For asthma patients age 2 to 18 year we utilized a modified discharge checklist to include identification of primary care provider (PCP), follow-up appointment made, medications receipt or confirmation of the ability to obtain medications after hospital discharge. A 24 multifactorial design matrix of the 16 bundle element combinations was developed by using 4 dichotomous (used/not used) factors. Study-It software was used to estimate and analyze each of the 4 factors effect and their interactions. Main effect terms and 2-factor interactions for each of the elements in the study were evaluated. Due to wide variation in subgroup size, weighted effect estimates were calculated and verified using statistical process control charts.
Results: Of 7730 subjects, 1277 were asthma patients (16.5%). Overall asthma RR was 2.6%. The number of subjects in each matrix category ranged from 15-254. The follow-up phone call connection rate was 45.5% (n = 585). The most effective single bundle element in reducing RR for asthma patients was the checklist (by 3.3%), followed by teach back reduced RR by 2.5%. Hand off to PCP’s reduced RR by 0.55%. In contrast, follow-up phone call increased RR by 2.2%.
Conclusions: This study confirms the importance of preparing families and patients with asthma for discharge by ensuring follow-up and availability of medications, as well as education about their condition. It also highlights the importance of the current trend in medication delivery to the bedside prior to discharge. The negative effect of the phone call may be related to the specifics of the population reached, as well as the possible identification of persistent symptoms by the caller promoting return to hospital for evaluation. The main limitation was the variation in number of patients in each bundle element combination of factors assessed. The next step will include a prospective analysis of effective elements. Further study is needed to elucidate the effect of the phone call.